Myelopathy is an injury to the spinal cord caused by significant pressure which results in neurological deficit. Neurological deficit is an impairment of mobility and function of a body area.
Myelopathy can occur in the cervical, thoracic and lumbar spine however cervical myelopathy is the most common. Lumbar myelopathy is very rare because for most people the spinal cord finishes at L1.
The symtoms are usually progressive, permanent and range from mild to severe and include:
Loss of balance and coordination
Abnormal, wide-based gait (difficulty with walking)
Loss of fine motor skills (eg. difficulty doing buttons and writing)
Altered sensation, pain and weakness in the limbs
Loss of bowel and bladder function
Paralysis
Death
Causes of Myelopathy
- Degenerative disease in the spine (wear and tear)
- Disc herniation
- Spinal stenosis
- Trauma
- Infection
- Tumours
- Autoimmune disorders including Rheumatoid arthritis
- Congenital disorders causing a narrow spinal canal
The combination of direct pressure on the spinal cord and ischemia (reduction of the blood supply) of the spinal cord leads to the spinal cord damage. Eventually the damage to the cord affects the patient’s neurological function. They may experience difficulty with balance and walk with an unsteady (ataxic) gait. A common funding is numbness particularly in the hands but also in the feet, as well as progressive difficulty in performing intricate functions such as doing up buttons or writing.
Myelopathy typically develops slowly however the progression of these symptoms is very variable between different patients and depends upon the degree of damage as well as the severity of the spinal cord compression.
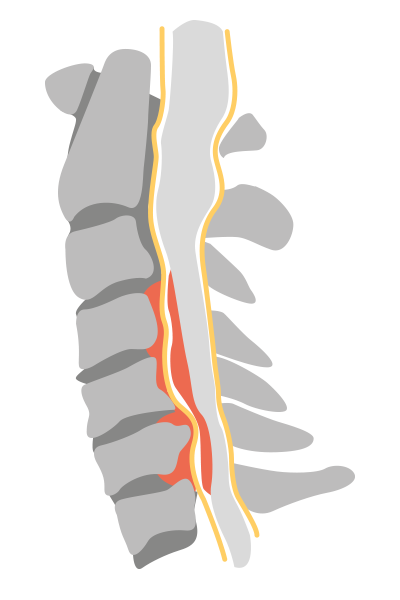

MRI scan showing the lateral view of a cervical spine where the cord is being compressed resulting in myelopathy. High signal (white) is seen within the cord at the levels of the compression.
Diagnosis & Treatment
How is it diagnosed?
The diagnosis depends on the age of the patient and therefore include other neurological problems such as multiple sclerosis.
Mr Hilton will take a detailed history and perform an examination of the nerves in the outpatient clinic to assess the severity of the cord damage.
Patients will require an MRI scan of the spine to confirm the diagnosis of myelopathy and to localise the position and extent of the problem. MRI scans show an increased signal (white on the scan) within the spinal cord which is consistent with a diagnosis of myelopathy.
Flexion/extension X-rays of the cervical spine are useful to exclude other causes and to assess if there is any instability of the spine, or kyphosis (excessive forward bending of the spine). This information is particularly important when planning surgery.
Surgery
The treatment for the cervical myelopathy is surgical decompression (surgically relieving the pressure on the spinal cord).
The decision to proceed to surgery depends on:
- The extent of the damage to the spinal cord
- The extent of the symptoms
- The speed of their deterioration
- And importantly, whether you want to have an operation.
Myelopathy symptoms vary greatly, in both the extent and speed of progression of the symptoms. The majority of patients will experience some progression of symptoms, but this may be very slow in certain individuals.
The aim of decompressive surgery is to relieve the pressure on the spinal cord and prevent further neurological damage to the spinal cord, unfortunately the nerves that have been damaged often do not recover. The timing of surgery is critical to prevent further neurological damage.
In some patients there are no symptoms or signs of neurological deterioration and so non-surgical management may be undertaken while regularly reviewing the patient in the out-patient clinic.
Surgery involves either decompression of the spinal cord from the front of the spine, with either, an anterior cervical discectomy and fusion, or if larger area of the cord is involved then a cervical verbrectomy (removal of one or more of the vertebral bodies) may be required.
Alternatively the spine can be decompressed from the back of the spine by either a laminectomy (the lamina is removed), or a laminoplasty, where the lamina is opened like a trap door.