What is Osteoporosis?
Bones are made up of a thin, solid outer covering with a trabecular inner part which looks like ‘honey-comb’. After the age of about 35 years, the amount of bone tissue we have naturally starts to reduce and the density of the trabecular bone decreases. This is described as ‘bone loss’ or ‘bone thinning’. Although our bones don’t look any different from the outside, the inner structure becomes thinner and a bit weaker – this is a normal part of ageing and is not osteoporosis.
In osteoporosis the bone density reduces too much and the bone is significantly weakened and the weakened bones are at a high risk for fracture. Osteoporosis is often called a ‘silent disease’ as there are no outward symptoms and the first sign of osteoporosis is usually a broken bone or fracture following minimal trauma. The bones most commonly fractured as a result of osteoporosis are the wrist, hip and spine.
About 3 million people in Britain have Osteoporosis and it results in an average of 300,000 fractures every year.
Osteoporosis itself does not cause pain however the broken bones caused by osteoporosis can be painful.
A vertebral compression fracture occurs when too much pressure is placed on a weakened, osteoporotic vertebra and the front of it cracks and loses height. Vertebral compression fractures are often the result of a fall, but people with osteoporosis can suffer a fracture even when doing everyday things, such as reaching, twisting, coughing, and sneezing. The fracture usually causes back pain around the fracture site although long-term back pain can be caused by the resulting change in the shape of the spine.
Risk factors for getting osteoporosis?
- Post-menopausal woman
- People who have had high-dose steroid treatment
- Family history of osteoporosis
- Being aged over 50 years
- Low body weight
- Malnutrition (including anorexia)
- People who have Crohn’s Disease, Rheumatoid arthritis and hyperthyroidism
- Calcium Deficiency
- Vitamin D deficiency
- Smoking
- Drinking excess alcohol
- Lack of exercise


This photo shows what ‘normal’ trabecular bone looks like


In osteoporosis, the density of the bone decreases and appears more ‘porous’

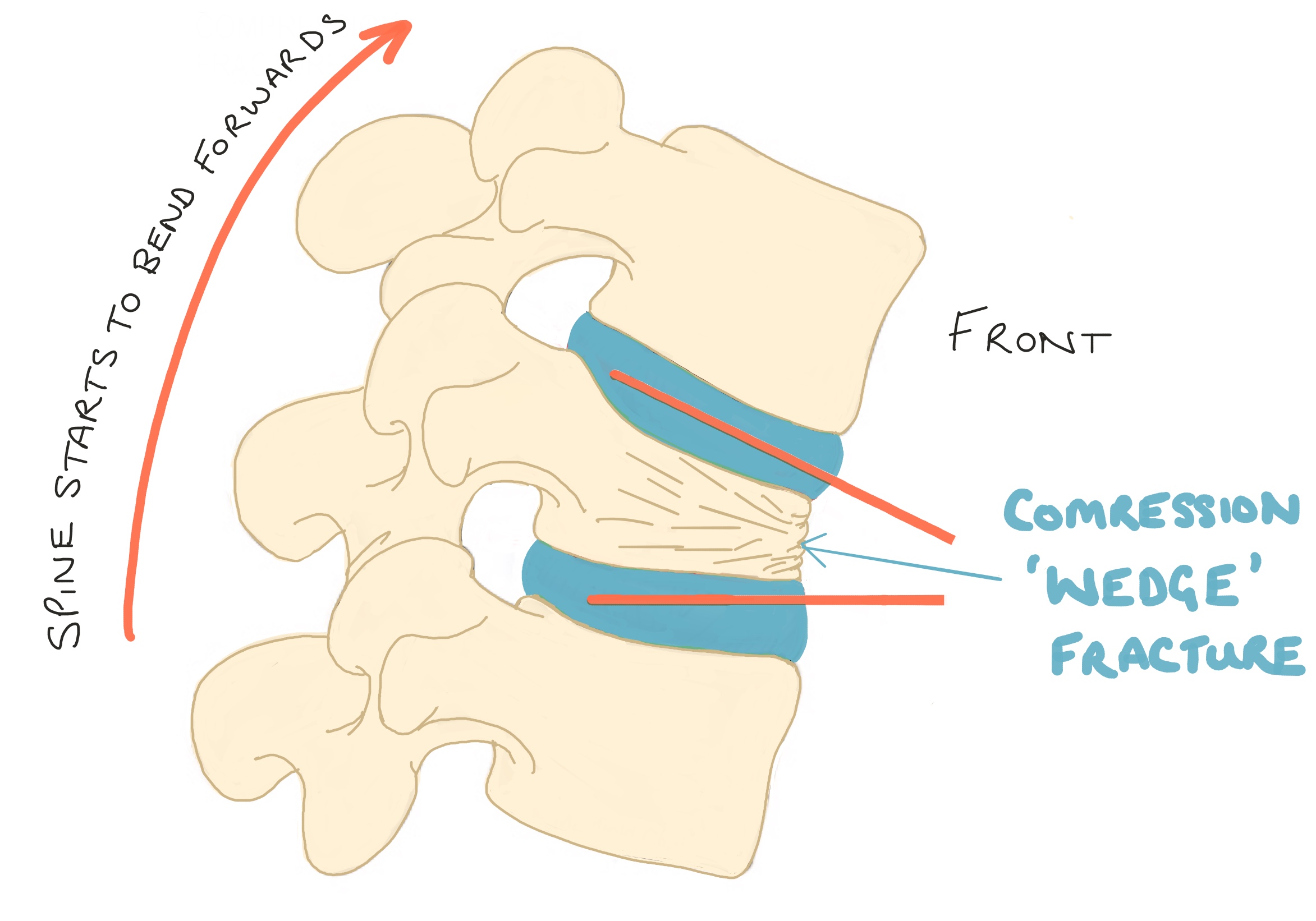
Diagram demonstrates a compression fracture; the front of the vertebral body is compressed resulting in the ‘wedge’ shape resulting in the spine starting to arch forward.
One fracture should not make much difference to the overall shape of the spine.
However, multiple vertebral fractures will result in a curvature of the spine, as seen in the MRI scan of the thoracic spine.


CT scan showing a L1 osteoporotic compression fracture.
CT scans are used to show fractures in more detail and are especially useful to assess the extent of the fracture and therefore the stability.

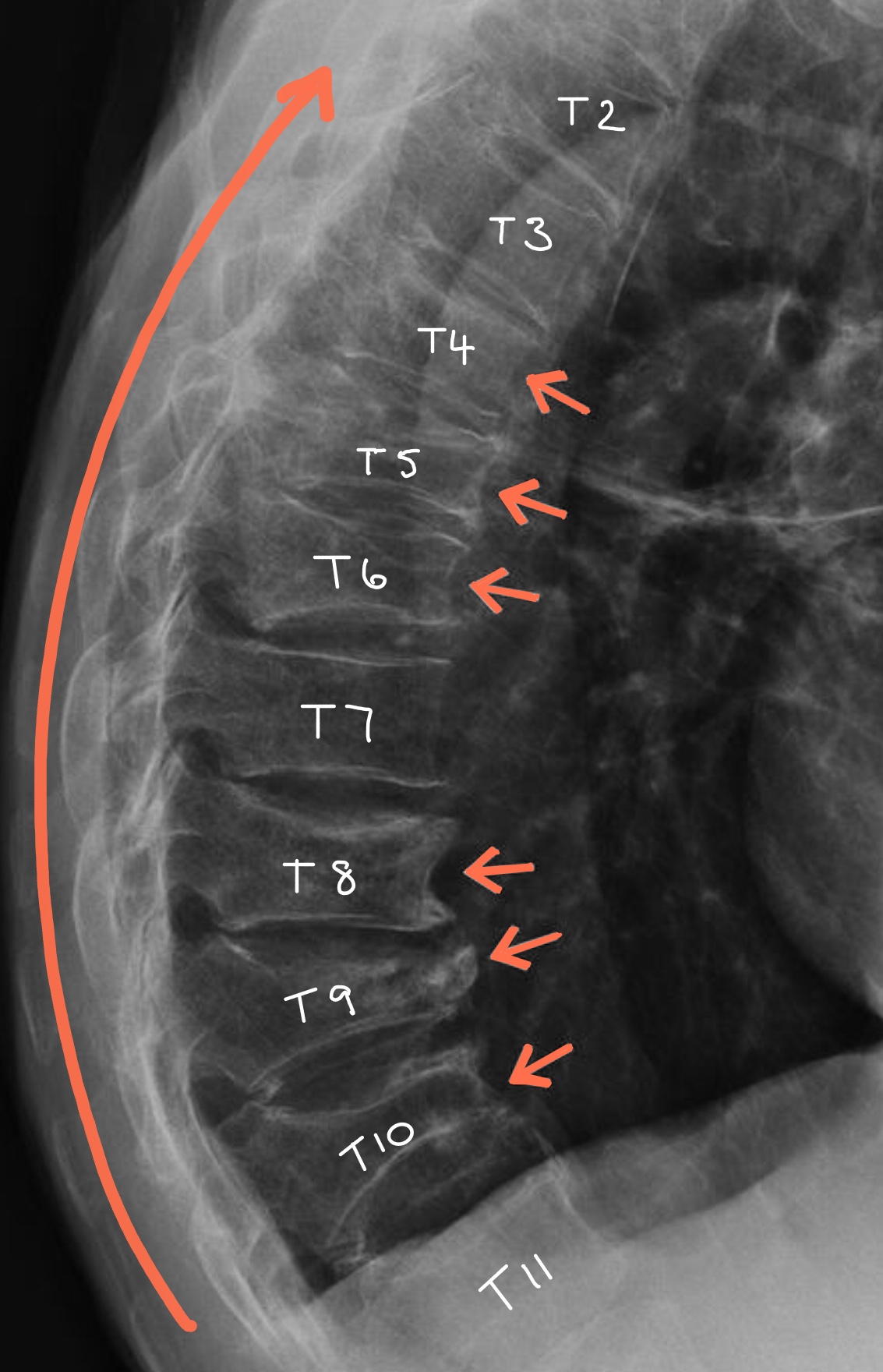
Multiple osteoporotic wedge fractures in the thoracic spine which causes a curvature called a ‘Dowager’s hump’.


MRI scan shows the same L1 fracture.
The high signal (white area) in the L1 body confirms that the fracture is unhealed and is probably a new fracture.
Osteoporotic Vertebral Fractures
The spine is made up of 33 small bones called vertebra, 24 of which are in the cervical, thoracic and lumbar spine and these are the bones which are most susceptible to osteoporotic compression fractures. Unlike other bones in the body, when an osteoporotic vertebra fractures it ‘squashes’ down on itself hence why it is called a ‘compression fracture’. The compression most commonly occurs in the front section, the ‘anterior column’, of the vertebra and this results in the bone becoming a ‘wedge’ shape. Occassionally, the middle and posterior columns of the vertebra also collapse and these fracture can be unstable and therefore are treated differently.
The most common fracture sites are the T12 and L1 (the ‘thoraco-lumbar juntion’) vertebrae. Unlike hip fractures, which almost always result from a fall, vertebral fractures often involve little/no trauma and no pain. As a result almost two-thirds of vertebral fractures have no symptoms. In fact they may go undiagnosed until they are seen on an x-ray taken for some other reason. Once a single fracture has healed there are usually no long-term consequences however statistically you are at higher risk of another fracture.
When a vertebral compression fracture heals it remains in the same compressed shape. Therefore one or two fractures are likely to produce a slight loss of height, but multiple fractures can contribute to a rounding of the back known as Dorsal Kyphosis or ‘Dowager’s Hump’. Once the fracture has healed the pain should improve, however due to the change in shape of the spine, unequal stresses on the facet joints and muscles may result in back ache. Occasionally, due to the loss of the vertebral height there maybe some irritation of the spinal nerves which may lead to pain or altered sensation in the area of the body which the specific nerve supplies.
Osteoporosis does NOT affect the healing process and, like all bone fractures, compression fractures take 6 – 12 weeks to heal however other factors may slow the healing for example, smoking and malnutrition.
Diagnosis
Osteoporosis is suspected if you have a fracture without much trauma and especially if you are female and over 50 years old. There are other possible diagnoses that can cause unexplained fractures, for example Multiple Myeloma and Tumours and these would also be investigated.
X-rays show the extent of the fracture and what treatment is indicated. X-rays can NOT diagnose osteoporosis or bone density.
For vertebral fractures, MRI and CT scans are sometimes performed to assess the age of the fracture and whether there is any spinal nerve compression.
A DEXA or ‘Bone Density’ scan will be performed and this shows the density of the bone. Bone density ranges from ‘Normal’ to ‘Osteopenic’ (borderline osteoporosis) and ‘Osteoporosis’.




Treatment Of Osteoporotic Fractures
Conservative Management
The majority of osteoporotic compression fractures occur in the anterior (front) part of the vertebral column and they usually heal naturally within 3 months without specific treatment to repair the fracture. Simple measures, such as a short period of rest and limited use of pain killers, are often all that is required. Often patients wear an extension brace to restrict movement, take the pressure off the spine and allow the vertebral compression fracture to heal. Some patients are referred for physiotherapy once their fracture has healed to help recondition and strengthen the core and postural stability muscles.
Surgical Treatment
In a few cases the vertebral fracture does not heal and/or the pain persists and further treatment maybe needed. The type of surgical treatment for osteoporotic vertebral fractures are kyphoplasty or vertebroplasty. The best candidates for these operations are patients who suffer severe pain from recent vertebral compression fractures. Mr Hilton can discuss whether a kyphoplasty may be suitable for you based on the type of vertebral compression fracture you have.
In a few rare cases, osteoporotic compression fractures can also involve the middle and/or posterior spinal columns as well as the anterior part. This type of fracture is potentially unstable and therefore usually requires surgical intervention to stabilise it.
Osteoporosis Treatment
“Prevention is better than cure”
A healthy, balanced diet and regular exercise is essential.
If you are at high risk of developing, regular DEXA scans are important and can be used to monitor the effectiveness of treatment.
If you are osteopenic or osteoporotic, you should discuss appropriate treatments with your doctor or osteoporosis specialist. Bone density, age and other risk factors are taken into account and medical treatment may include:
Calcium and Vitamin D Supplements
Bisphosphonates
Selective Oestrogen Receptor Modulators (SERMs)
Hormone Replacement Therapy (HRT)
Parathyroid Hormones