Spondylolisthesis means the abnormal slip of one vertebra with respect to the vertebra immediately below.
In Latin “spondylo” means spine and “listhesis” means slippage.
The slippage of the upper vertebra with respect to the vertebra below can be in three different directions. Most commonly, the slip of the upper vertebra is in the forwards direction (anteriorly) and this is called an anterolisthesis. Less common is a backwards (posterior) slip, also known as retrolisthesis. Much less common is a sideways (lateral) slip, called a laterolisthesis.
There are four grades of severity of slip, determined by the amount that the upper vertebra has slipped in relation to the lower one:
Grade 1: a slip of less than 25%
Grade 2: 25-50% slip
Grade 3: 50-75% slip
Grade 4: 75-100% slip
What causes a spondylolisthesis?
Most common causes:
1) Degenerative Spondylolisthesis
This type of slip is due to degeneration of the pair of facet joints between the two affected vertebrae. Degenerative spondylolistheses usually occur in older women and most commonly occurs at L4/5. It is virtually never worse than grade 1, as in the MRI scan on the right.
The slip may cause either low back pain and / or symptoms related to nerve compression, which include pain, weakness, numbness/altered sensation or tingling in one or both of the legs. The area affected depends upon which of the nerves is being compressed because different nerve roots map out different areas on the body.
2) Lytic or Spondylolytic Spondylolisthesis
This is due to a “pars defect” which is a small break or stress fracture in the bone that connects the facet joints. As a result they can become separated which is also called “Spondylolysis”. The upper vertebra is unable to maintain its correct position and slips out of place causing a spondylolisthesis. See section on Pars Defects in Conditions.
Lytic spondylolisthesis usually occur at the L5/S1 level and normally present in the teenage years and 20s. They predominantly seen in high achieving athletes and certain sports can cause a pars defect by causing repetitive stress on the vertebra by constantly over stretching it on one or both sides and usually occurs with no history of trauma. Typical sports associated with pars defects are gymnastics, ballet dancers, rowers, weight lifting, fast bowlers in cricket, field athletics, rugby players and tennis players.
3) Dysplastic (congenital) Spondylolisthesis
Some people are born with abnormal or ‘dysplastic” facet joints. During foetal development Occassionally abnormal bone formation of one (or more) of the vertebrae occurs and this can result in the vertebrae not being able to maintain their normal alignment and the slip out of position. This does not always cause symptoms as the body get can used to the abnormal position of the vertebrae however the abnormal arrangement of the vertebrae puts them at greater risk for slipping and causing irritation and compression of the nerve roots.
Less Common Causes:
4) Post-Traumatic Spondylolisthesis
This is due to an injury/trauma that causes a spinal fracture or slippage of the vertebrae.
5) Pathological Spondylolisthesis
This happens when the spine is weakened by disease for example by a tumour, a spinal infection or osteoporosis. The weakened, disease bone fractures and is unable to maintain its correct position.
6) Iatrogenic Spondylolisthesis
Iatrogenic means it has been ‘caused by medical treatment’ and in this case it refers to a slippage that occurs or becomes worse after spinal surgery. In decompression operations too much bone and soft tissue can be removed and as a result the segment becomes unstable and slips out of position. This does not necessarily mean the intial surgery was performed wrong or done badly but it does usually mean another operation maybe needed to stabilise the segments.
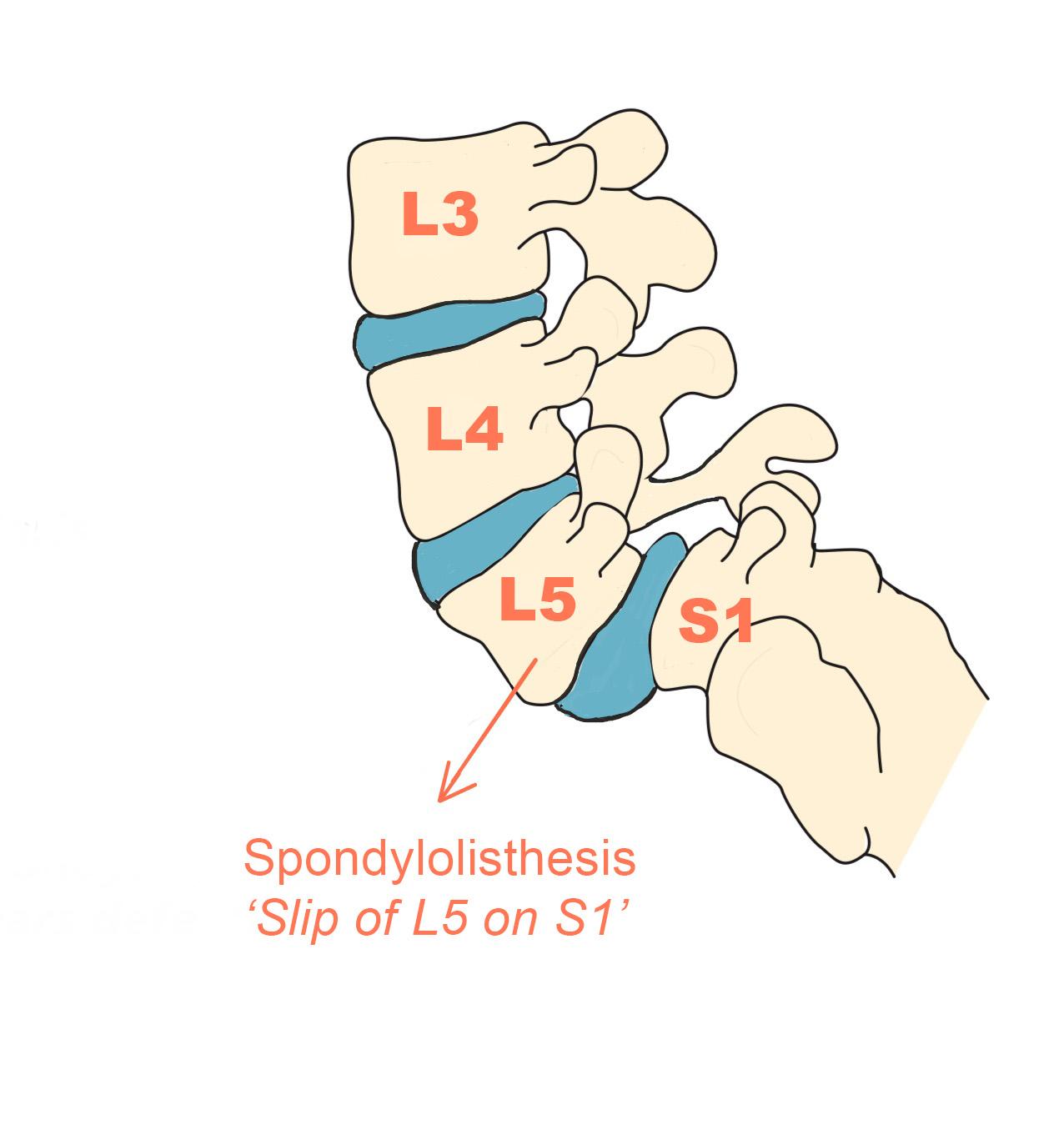
The diagram shows a forward slip or “anterolisthesis” of the L5 vertebra over the S1 vertebra.

The MRI image shows a grade 1 anterolisthesis (a forward slip of less than 25%) of L4 on L5.
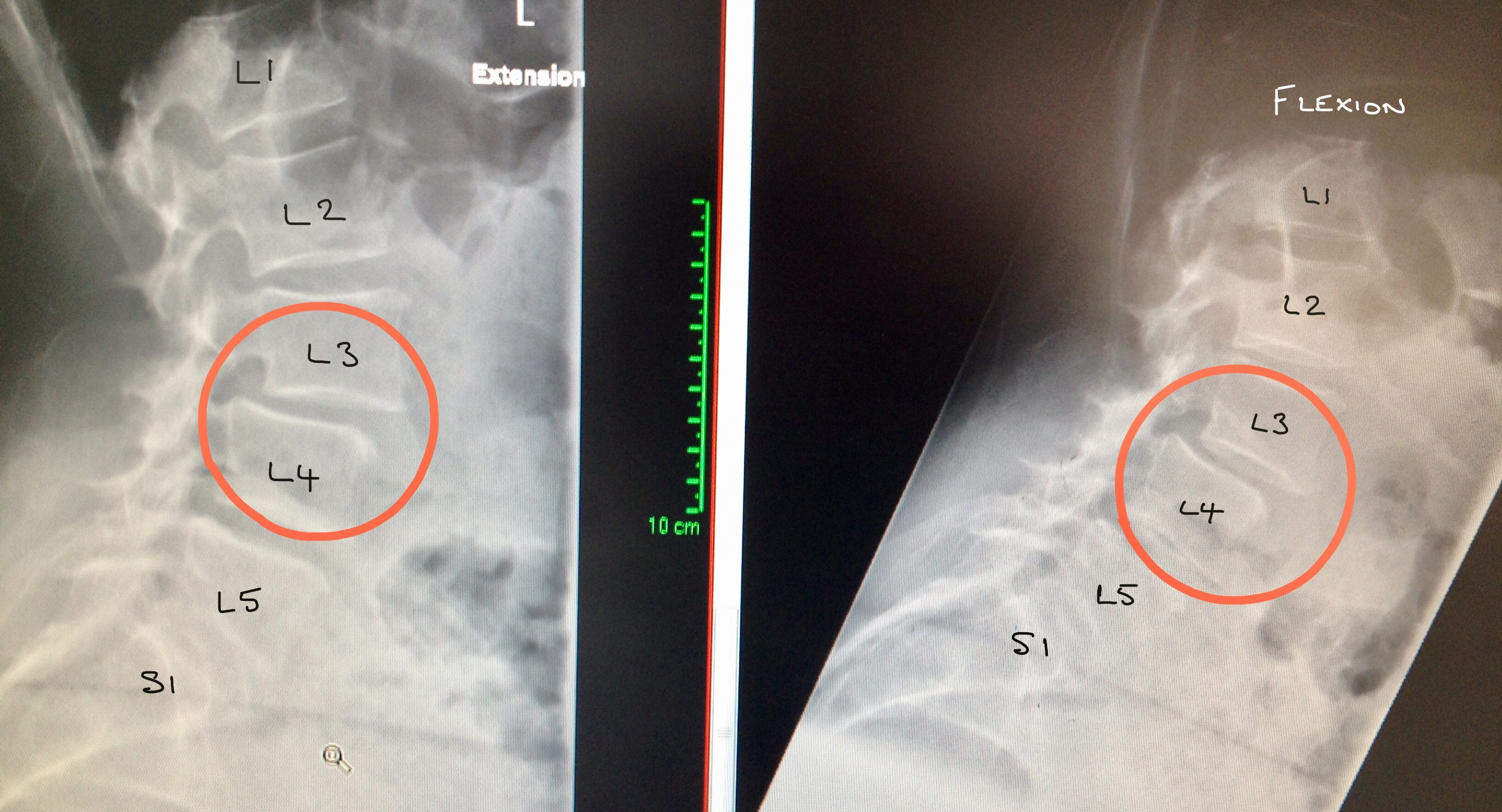
Flexion/extension X-rays demonstrating instability of the L3/4 anterolisthesis.
Diagnosis
Mr Hilton always takes a detailed history and performs a neurological examination as the first of any diagnosis process. Imaging is used usually to confirm, or exclude, a diagnosis and this is generally in the form of standing X-rays and a MRI.
Flexion and extension X-rays are performed to assess the stability of the vertebrae, especially at the level of the spondylolisthesis.
Treatment
Treatment options then depend upon the severity and duration of the symptoms as well as the underlying cause.
Conservative Management and Physical Therapy
Improving spinal mobility, core muscle strength and overall fitness is essential and may improve the pain to a manageable level.
Simple painkillers, using over the counter medication such as paracetamol or anti-inflammatories, eg. Ibuprofen, maybe helpful not only to relieve the pain but also help you to perform your physiotherapy exercises.
The stronger your core and postural stability muscles are, the more support and protection your spine has against the stresses and forces placed on the spine.
Lifestyle changes may also effectively help your manage the symptoms.
Spinal Injections
X-ray guided epidurals and nerve root injections can be extremely useful in patients to help to relieve leg pain (and sometimes altered sensation) caused the irritation of the spinal nerves. They are also very useful in the diagnostic process and can help confirm or exclude a diagnosis.
Spinal injections are performed under local aneasthetic or sedation and although there are potential risks and side effects, these are extremely rare. See section on spinal injections for more information.
Surgery
Surgery, in the form of a lumbar decompression with or without an instrumented fusion, is considered when the pressure on the nerves causes severe leg pain and all conservative measures have been exhausted or if there is progressive weakness.
Surgery for back pain alone is usually not considered as per the current NICE guidelines.
As with all causes of cauda equina syndrome, emergency decompression is indicated if there is loss of bowel, bladder or sexual function.