Just like anywhere else in the body, infections can occur in the spine; in the spine an infection of the intervertebral discs is most common but infections of the bones and in the epidural space may occur.
Spinal infections are usually caused by either a bacterial or fungal infection in another part of the body being carried to the spine by the bloodstream. The most common spinal infection is caused by a bacteria called Staphylococcus aureus, followed by Escherichia coli. However infections in the spine can be a complication of a surgical procedure although this is rare.
Although infections in the spine are rare they are serious and require urgent treatment.
What are the risk factors for developing a spinal infection?
- Diabetes
- Smoking
- Immunosuppression (either from acquired immunodeficiency syndrome or medical treatment for tumors)
- Malignancy
- Organ transplantation
- IV Drug use
- Recent urinary tract instrumentation
- Spinal surgery
- Malnutrition

Microscopic photo of Staphylococcus aureus, the most common bacteria to cause infections in the spine.

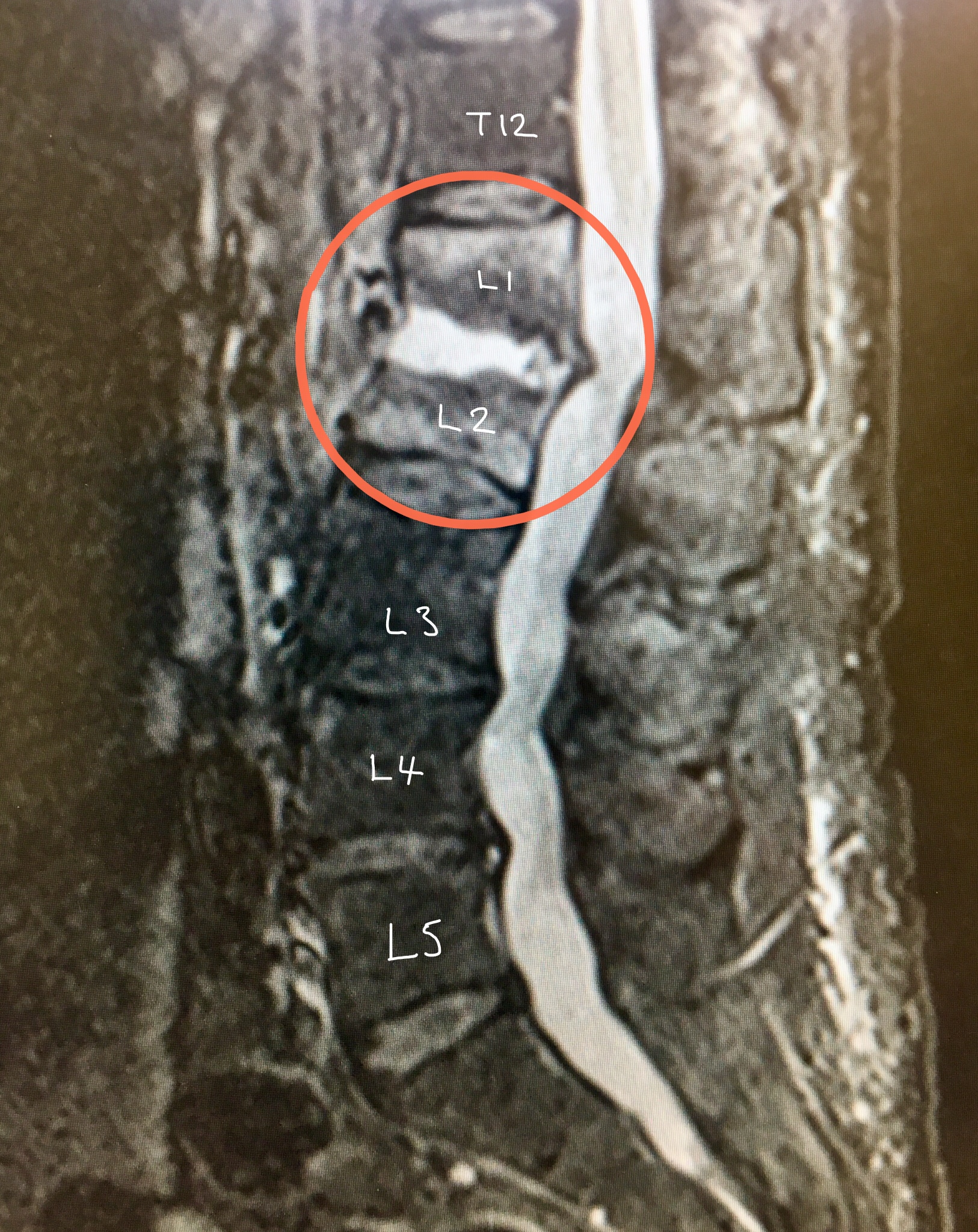
MRI scan with STIR shows an infection in the L1/2 disc (appears white) and the adjacent vertebrae which look whiter than the other vertebrae.

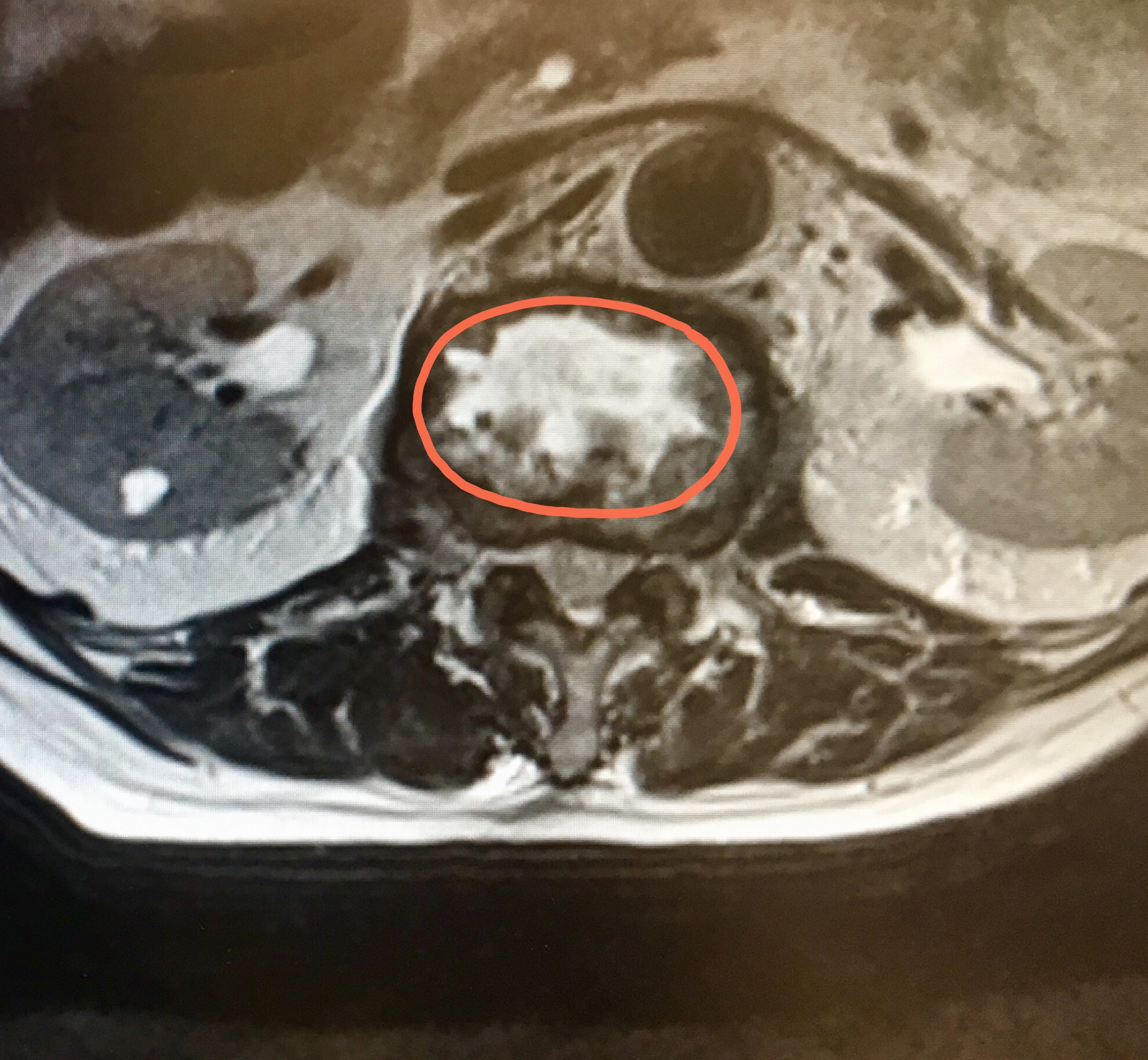
Cross-section MRI view of the L1/2 disc – the white area represents the infection
Symptoms
Patients often become generally unwell, starting with flu-like symptoms and get sudden onset, constant back pain that does not go away with rest. However the symptoms maybe much more subtle, the person may not feel unwell and this often leads to a delay in diagnosis. Some patients may also develop pain or altered sensations in their arms or legs (depending where the infection is in the spine).
Diagnosis
Spinal infections should be suspected as a possible diagnosis in patients with sudden onset, relentless and progressive symptoms who have no history of trauma and especially if they have a fever and/or the above risk factors. Therefore a careful history and examination is essential.
Blood tests may confirm an infection – these include a full blood count (FBC) and inflammatory markers of infection, CRP and ESR. However some patients do not have any changes in their inflammatory markers, this is especially common in patients who are immunosupressed.
MRI scan with STIR sequence can show where the infection is located and the extent of the infection.
A CT guided biopsy 9or aspiration) is very useful in order to get a sample of infected spinal tissue that is sent to the microbiology laboratory for “cultures and sensitivities” – this identifies the pathogen (“bug”) causing infection. A diagnosis may then be made when the specific pathogen is known and the most appropriate antibiotic treatment can be started. Patients are initially started on ‘broad-range’ intravenous (IV) antibiotics before the microbiology results are back as these can be altered if necessary.
Treatment
The first line treatment of spinal infections is to treat the infection with appropriate IV antibiotics for at least 6 weeks. If after 6 weeks of IV antibiotic treatment, the inflammatory markers of infection in the blood (CRP and ESR) have normalised then the treatment is usually changed to a 6 week course of oral antibiotics. However, if the inflammatory markers in the blood are not normal after 6 weeks the IV antibiotics are usually continued until they are normal. Antibiotic choice and duration of treatment is also usually guided by a Consultant Microbiologist.
Very occasionally, surgery maybe needed for:
- Progressive neurological impairment i.e. paralysis
- Some spinal abscesses
- Progressive spinal deformity
- Infection causing spinal instability
- Failure of non-operative treatment
Surgery for infection usually involves excising the dead bone and infected tissue and possibly stabilising the spine with screws and cages.


Recovery
Although it is a long process, once the treatment has started the back pain should gradually improve. The infection will cause some destruction of the disc and/or bone and therefore there will long term changes seen on future imaging. Often the changes eventually lead to a fusion of the vertebrae. However once the infection has been successfully treated been there should minimal pain although some people may continue to experience long term back ache due to the change in shape of their spine.