Kyphoplasty is a minimally invasive surgical procedure that is used to treat pathological fractures of the vertebrae due to osteoporosis, cancer, or benign tumours.
The aim of a kyphoplasty surgical procedure is to improve the pain caused by a spinal fracture, to prevent further collapse and to restore the lost vertebral body height caused by the compression fracture.
Kyphoplasty is considered for osteoporotic fractures if conservative management has failed and the compression fracture remains unhealed and is very painful.
What is a vertebral compression fracture?
Vertebral compression fractures most commonly occur as a result weakened bone structure caused by osteoporosis.
As part of the normal ageing process our the inner structure of our bones becomes thinner and a bit weaker – this is not osteoporosis. In osteoporosis the bone density reduces too much and the bone is significantly weakened and the weakened bones are at a high risk for fracture. Osteoporosis is often called a ‘silent disease’ as there are no outward symptoms and the first sign of osteoporosis is usually a broken bone or fracture following minimal trauma. The bones most commonly fractured as a result of osteoporosis are the spine, wrist and hip.
A vertebral compression fracture occurs when too much pressure is placed on a weakened, osteoporotic vertebra and the front of it cracks and loses height. Vertebral compression fractures are often the result of a fall, but people with osteoporosis can suffer a fracture even when doing everyday things, such as reaching, twisting, coughing, and sneezing. The fracture usually causes back pain around the fracture site although long-term back pain can be caused by the resulting change in the shape of the spine.
Diagnosis
An osteoporotic vertebral compression fractures are suspected if there was minimal trauma associated with the fracture in women over 50 years old. There are other possible diagnoses that can cause unexplained fractures, for example multiple myeloma and metastatic tumours, including those arising from breast or lung cancer, or lymphoma. Benign lesions include hemangioma and giant cell tumor. These alternative diagnoses should be thoroughly investigated.
X-rays show the extent of the fracture and what treatment is indicated. MRI with STIR and CT scans are performed if the pain persists despite, normal conservative management, to assess the age of the fracture and whether there is any spinal nerve compression.
X-rays can NOT diagnose osteoporosis or bone density.
If considering treatment with a kyphoplasty, an MRI scan with STIR sequence will be performed to confirm the fracture is unhealed and to assess whether a kyphoplasty is possible and therefore an option.
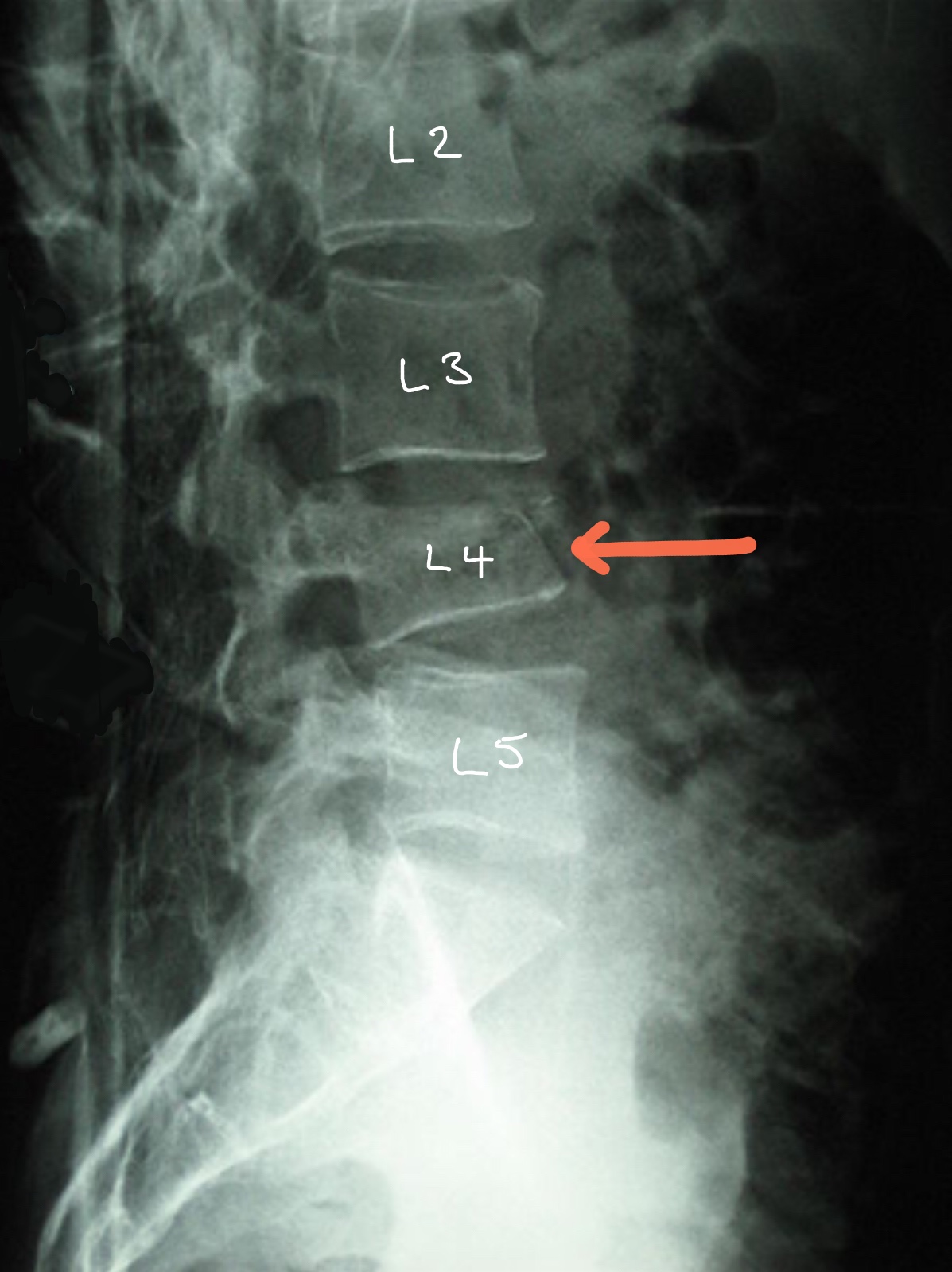
X-ray showing a compression ‘wedge’ L4 fracture – from this X-ray the age of the fracture and whether it is healed is unknown

MRI scan confirms an unhealed compression L1 fracture.
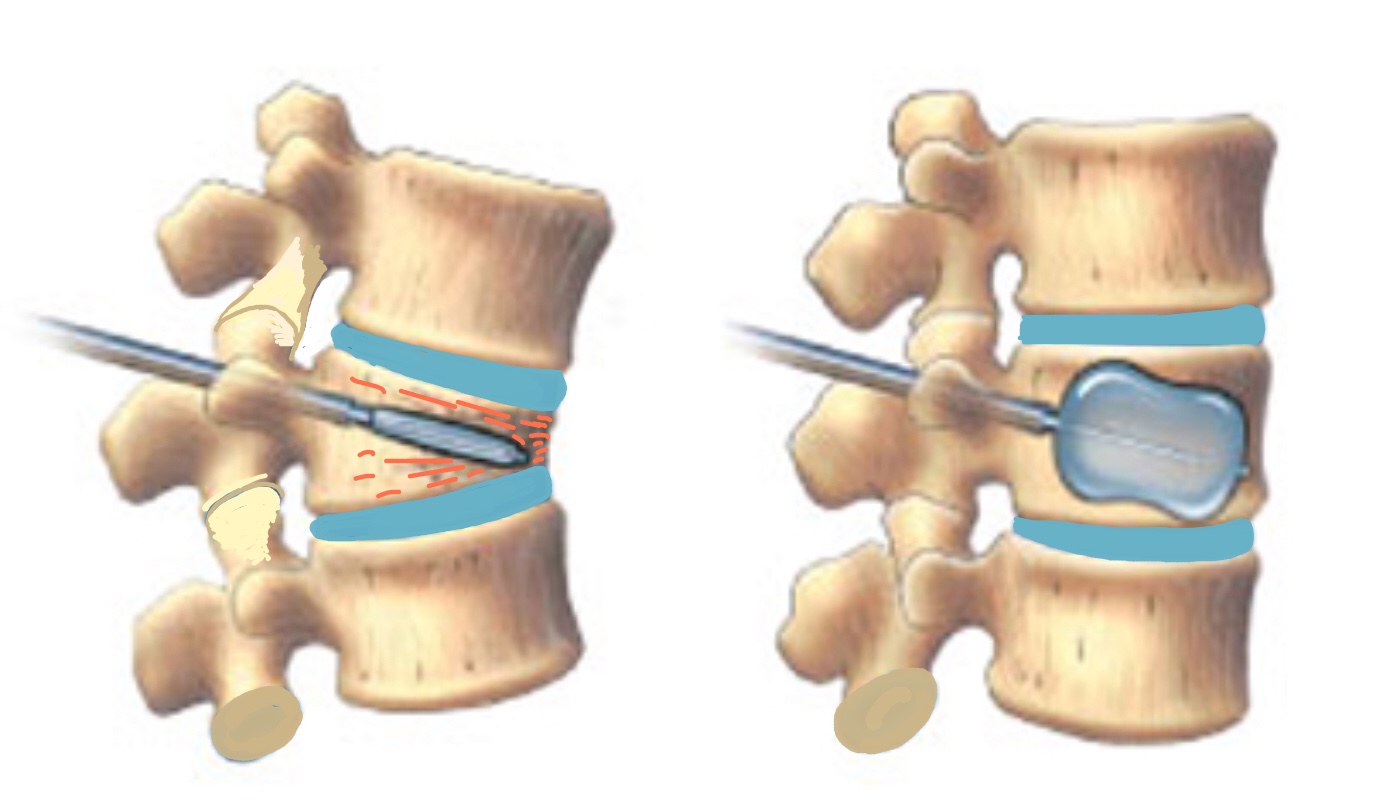
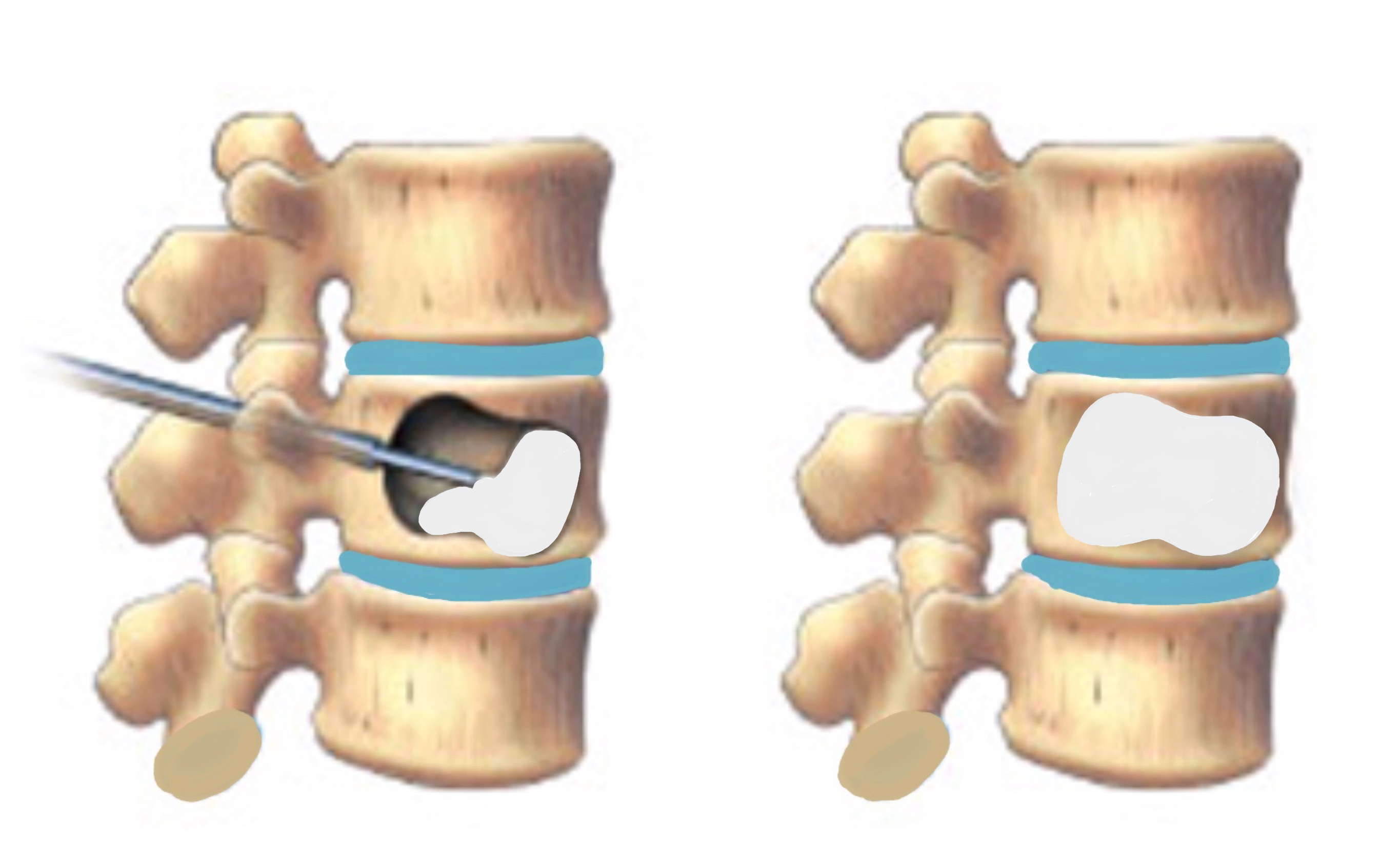
The diagrams demonstrate steps 1 – 5 of the procedure
The Kyphoplasty Procedure
The procedure is performed in theatre under X-ray guidance. Although the procedure is minimally invasive it is still performed under general anaesthetic and usually requires an overnight stay in hospital.
During the procedure:
- A tube is inserted through two 1cm cuts in the back into the damaged vertebrae. X-rays are used throughout the procedure to help ensure the accuracy of the procedure.
- A thin balloon catheter tube is guided into the vertebra.
- The balloon is inflated to create a cavity in which liquid bone cement is injected.
- The balloon is then deflated and removed.
- Special bone cement is injected into the cavity which hardens in about 10 minutes.
Risks and Complications of Kyphoplasty
- Infection
- Bleeding
- DVT/PE
- Cement leakage into the spinal canal which can cause paralysis and major nerve damage
- Cauda Equina Syndrome
- Irritation or damage to other structures, including the spinal cord
- Failure to relieve pain/symptoms
- Medical complications including heart attack (MI), stroke (CVA) and death.
Less than 1% of patients experience complications from kyphoplasty.
Recovery
Most patients feel almost instant pain relief when they wake up but this is not always the case so do not worry. Although about 5% of patients feel there are no change in their pain symptoms following a kyphoplasty despite the vertebral body height has been restored.
Following the procedure patients are able to mobilize without restrictions and the majority of patients are discharged from hospital within 24 hours of the procedure.
Mr Hilton or one of his team will see you at about 7 – 10 days following your operation to check your wounds and also to see how you are getting on. All patients are advised NOT to change their dressings. You are at risk of getting a wound infection if you change your own dressing.
If you are concerned about your wound or you feel it is necessary to change the dressings before your wound check appointment, then either:
Place a fresh dressings over the top of the original dressings
OR
Contact the hospital or your GP practice.