‘Fusion’ in spinal surgery means joining two bones solidly together and therefore preventing any movement in the future between the bones. Mr Hilton regularly performs posterior lumbar spine fusions in the treatment of leg and back pain when there is instability between two vertebrae.
Instability of the spine may result in a spondylolisthesis, movement of one vertebra relative to the adjacent vertebra, which may lead to back pain or pressure on the nerves, which may cause leg pain. The spondylolisthesis may be reduced and fused, or under certain circumstances, fused in its slipped position.
Spondylolisthesis means the abnormal slip of one vertebra with respect to the vertebra immediately below.
The slip may cause either low back pain and / or symptoms related to nerve compression, which include pain, weakness, numbness/altered sensation or tingling in one or both of the legs.
What is an instrumented fusion?
A spinal fusion is an operation that is used to stabilize the spinal vertebrae. The aim of a lumbar fusion is to create a solid bridge of bone between two or more vertebrae and provide stability. Spinal fusion is considered when there is a significant loss of disc space or the spine is unstable.
Lumbar decompression surgery is used to first used to relieve the pressure on the nerves within the spine. If the spine is unstable or if there is a spondylolisthesis then the decompression may be combined with a spinal fusion.
There are different techniques used to achieve the fusion and this can be related to both the type of metalwork used and where the bone graft is placed.
1) Postero-lateral Fusion: bone graft is placed at the back of the spine (posteriorly) and next to the transverse processes of the vertebrae (lateral) and maybe stabilised with or without metal instrumentation.
2) Interbody Fusion: Bone graft placed in a cage between the vertebra (in the space where the disc has been removed) and always stabilised with metal instrumentation.
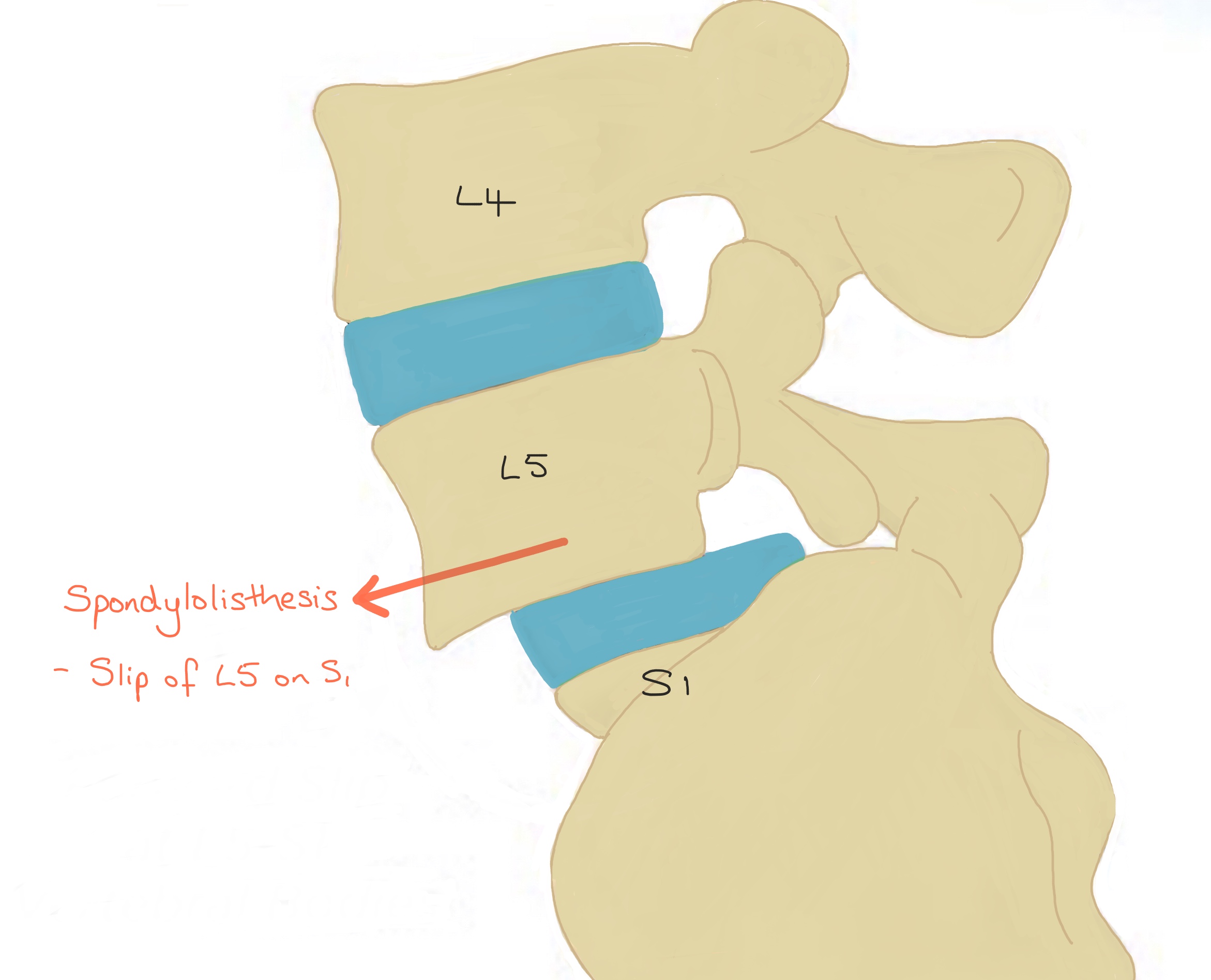
Diagram showing an anterolisthesis at L5/S1 causing instability which, if symptomatic, would require a decompression and an instrumented fusion.
The different types of Posterior Fusions
Before deciding on the exact type of operation and system Mr Hilton will use, several factors are taken into consideration including how narrow the nerve canal has become and how much the vertebra has slipped.
Whatever the type of fusion technique, the first part of the operation involves a decompression; the intervertebral disc and any tissues irritating the nerves are removed. The interbody cage is then fitted into part of the space created between the two vertebrae and the rest of the space is packed with bone graft. The bone graft is usually the bone that is initially removed from the vertebrae at the beginning of the operation and therefore it is the patients own bone. Although, if there is not enough of the patients bone, some synthetic bone substitute may also be used.
Lumbar fusion surgery is performed predominantly for the relief of leg pain and/or weakness.
In 70% of the patients their pain will be at least halved, in 25% of patients there will no change in their level of pain and in 5% the symptoms maybe worse.
1) Posterior Lumbar Interbody Fusion (PLIF) using Pedicle Screws, Rods and Cage
The first part of the operation involves a decompression; the intervertebral disc and any tissues irritating the nerves are removed. The interbody cage is then fitted into part of the space created between the two vertebrae and the rest of the space is packed with bone graft. The bone graft is usually the bone that is initially removed from the vertebrae at the beginning of the operation and therefore it is the patients own bone. Although, if there is not enough of the patients bone, some synthetic bone substitute may also be used.
The ‘cage’ (or ‘implant’ as it is sometimes called) is either made of titanium or trabecular metal and although it looks like a solid block on the X-rays, it is actually porous to allow bone to grow into it and becomes incorporated into the fusion. Cages come in different sizes to fit the space between your vertebrae perfectly and either one or two cages can be implanted.
After the decompression and positioning of the cage, the pedicle screws are placed into the pedicle of the vertebra on both sides, above and below the unstable spinal segment. These screws act as firm anchor points to which rods can be connected. The screws and rods act as an internal scaffolding that provides a solid structure to allow a solid bone fusion to take place. Once the bone fusion is complete the scaffolding is actually no longer required but most surgeons do not recommend it is removed unless it actually needs to be which is rare.
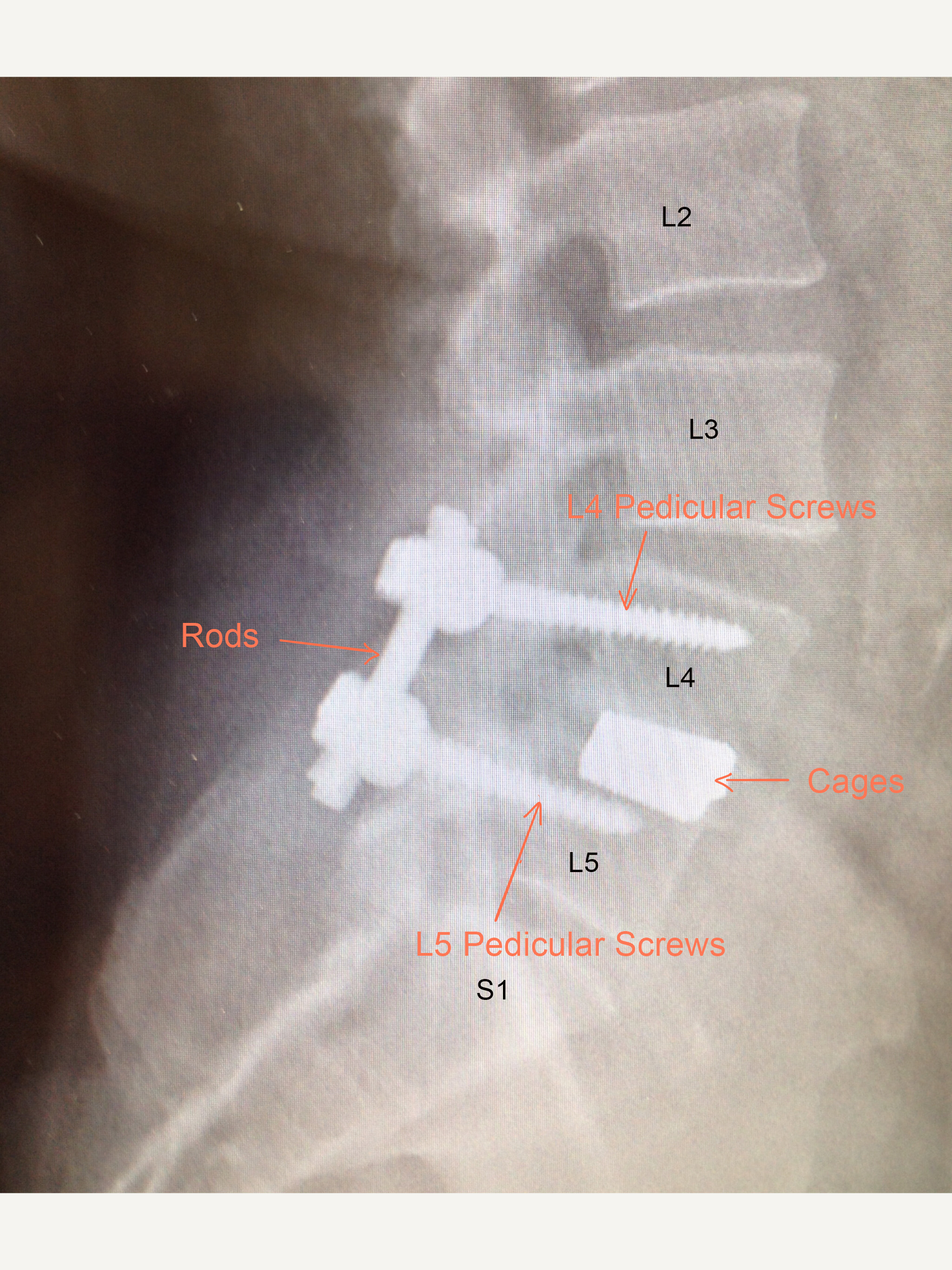
Lateral view X-ray showing the position of the pedicle screws, rods and cages at the L4/5 PLIF.
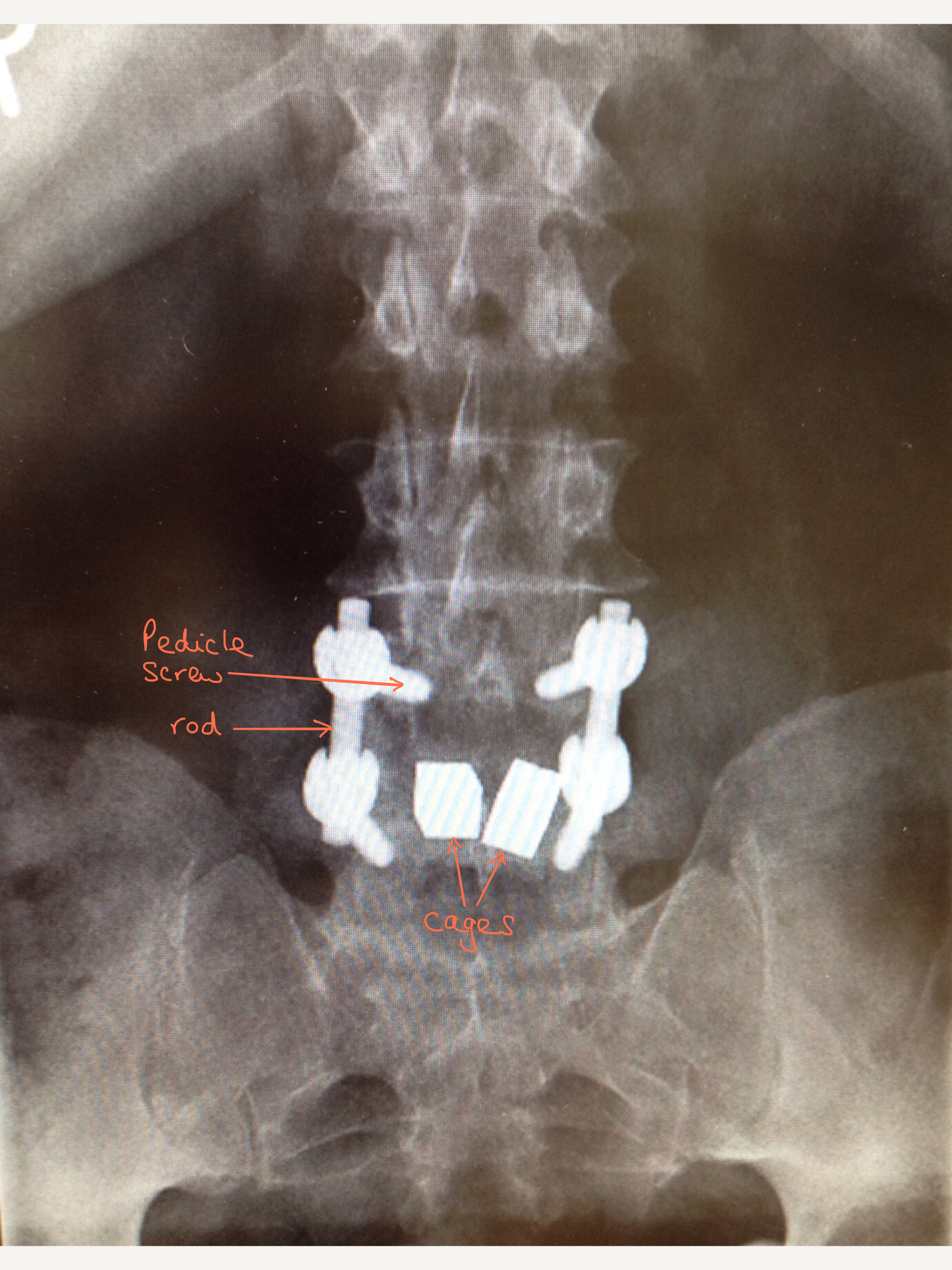
Front view (AP) X-ray of the position of the PLIF metalwork. In this type of fusion two cages are placed in the decompressed disc space.
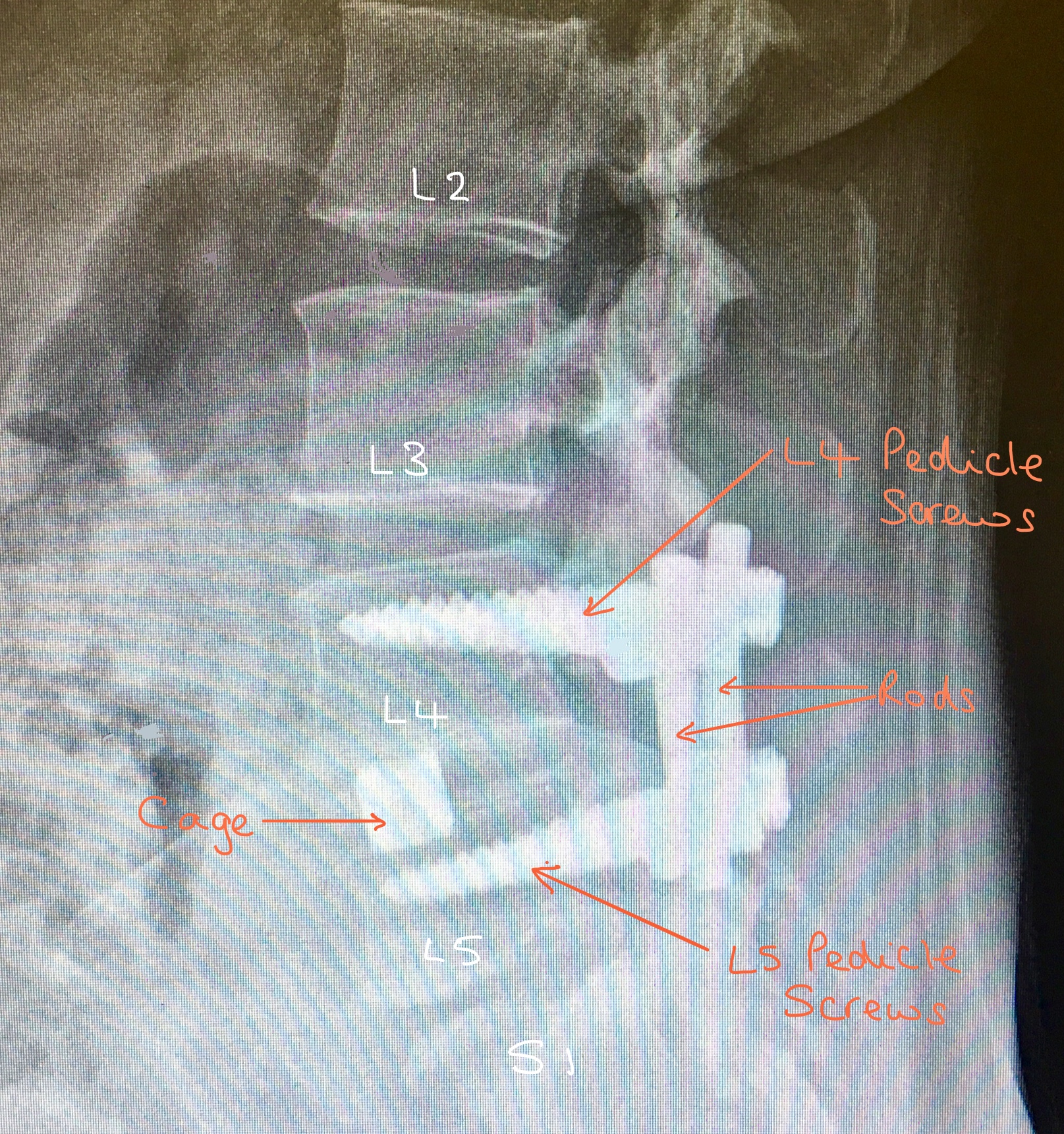
Lateral view X-ray showing the position of the pedicle screws, rods and cage in a L4/5 TLIF.
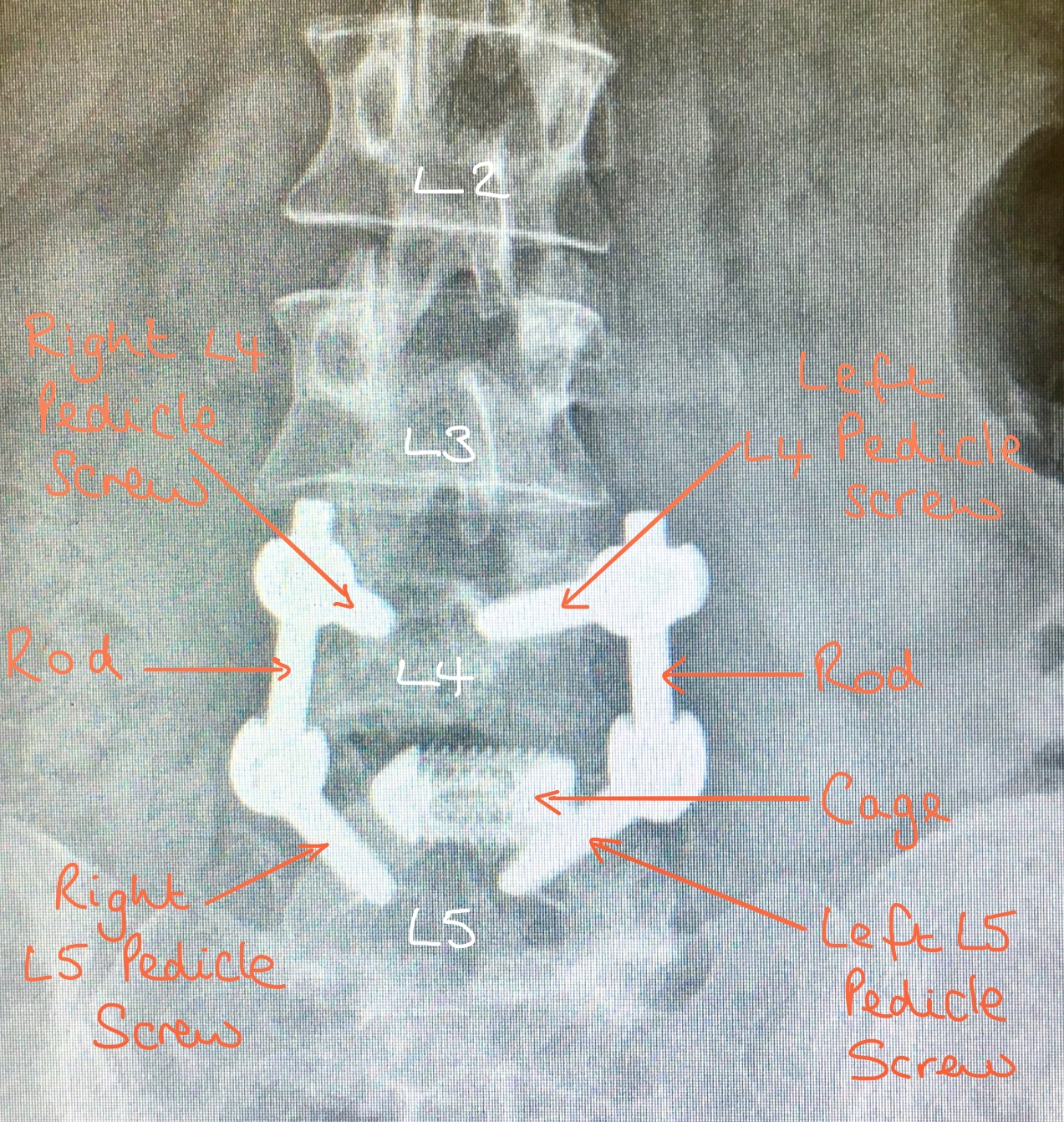
Front view (AP) X-ray of the position of the metalwork in a TLIF. In this type of fusion one cage is placed in the decompressed disc space.
2) Transforaminal Lumbar Interbody Fusion (TLIF) using screws, rods and a cage.
This type of fusion is very similar to a PLIF (as described a bove) but the surgical approach is different; in a PLIF the approach is more from the middle of your back whereas in a TLIF the approach is from the side (unilateral) via the ‘foramen’ and hence, typically only one cage is put into the intervertebral disc space.
When deciding whether to perform a PLIF or a TLIF, Mr Hilton takes into consideration a patients anatomy and symptoms. Although they are technically different operations, the end result of a fusion is the same.
Pedicle screws are inserted into the vertebra in a similar way as in a PLIF however at a slightly different angle. The facets joints at the back of the spine are then removed and the intervertebral disc between the vertebral bodies is removed. A single nerve root is then temporarily moved out of the way to protect it whilst the cage, packed with bone graft, is placed between the vertebrae.
As with a PLIF, the pedicle screws are then connected together with the rods and then more bone graft is placed between the transverse processes of the vertebral bodies, to obtain a fusion.
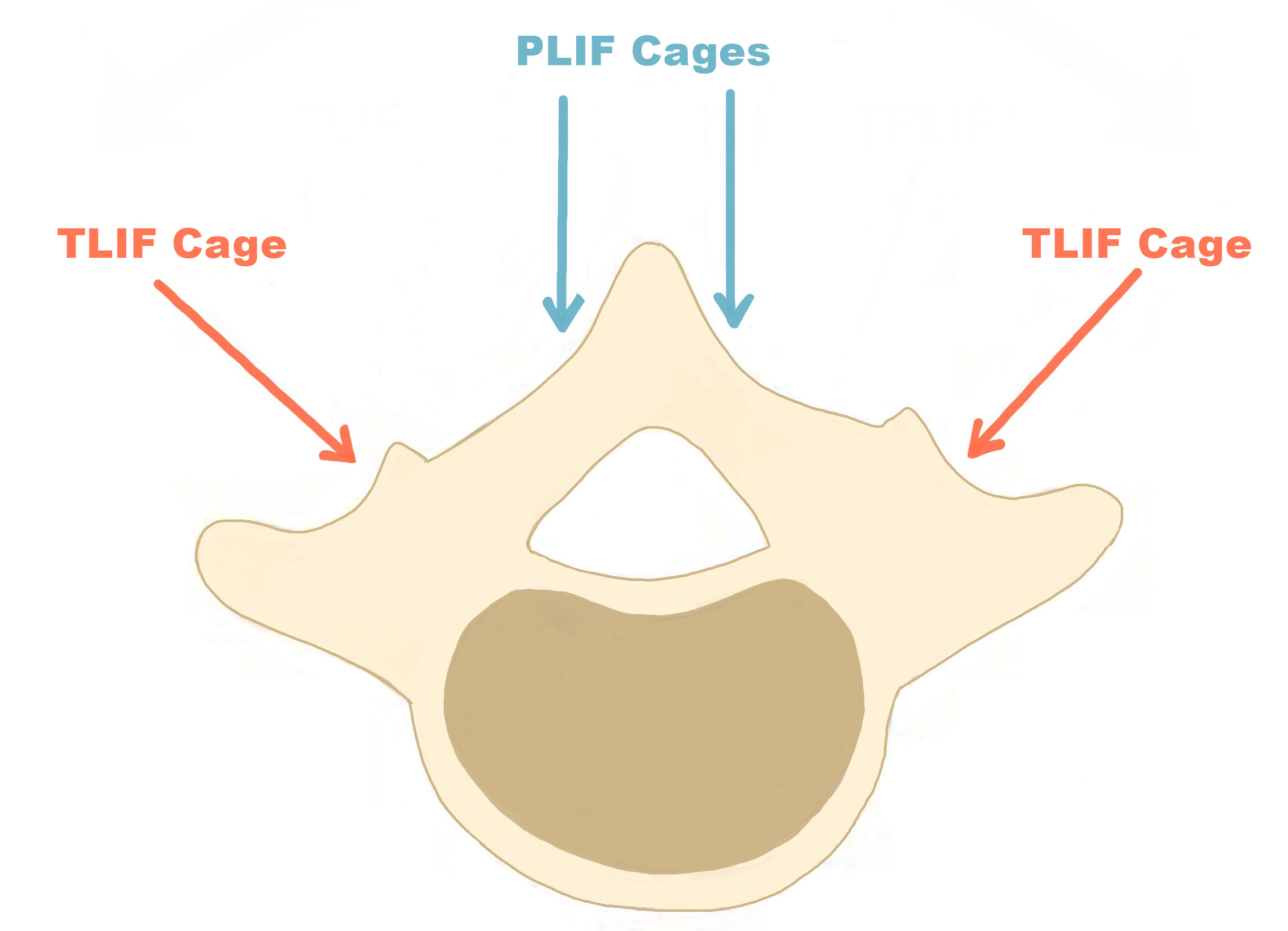
The diagram demonstrates the different surgical approach placing the cage in PLIFs and TLIFs
3) Posterior Lumbar Fusion
The difference between this type of fusion and the other posterior fusions is no intervertebral cage is used. Instead bone graft is placed between the transverse processes of the two vertebrae. There are two boney transverse processes on either side of the vertebra that stick outwards.
As with the other fusions, the bone graft will heal after several months and should produce a solid fusion between adjacent vertebral bodies within the spine. In order for the bone to fuse, the spine is stabilised with screws and rods which act as an internal scaffold.
One of the main reasons for performing a posterior lumbar fusion without inserting a cage between the vertebrae is because the space between the vertebrae is reduced so much (usually due to wear and tear/degeneration) that a cage cannot safely be inserted.
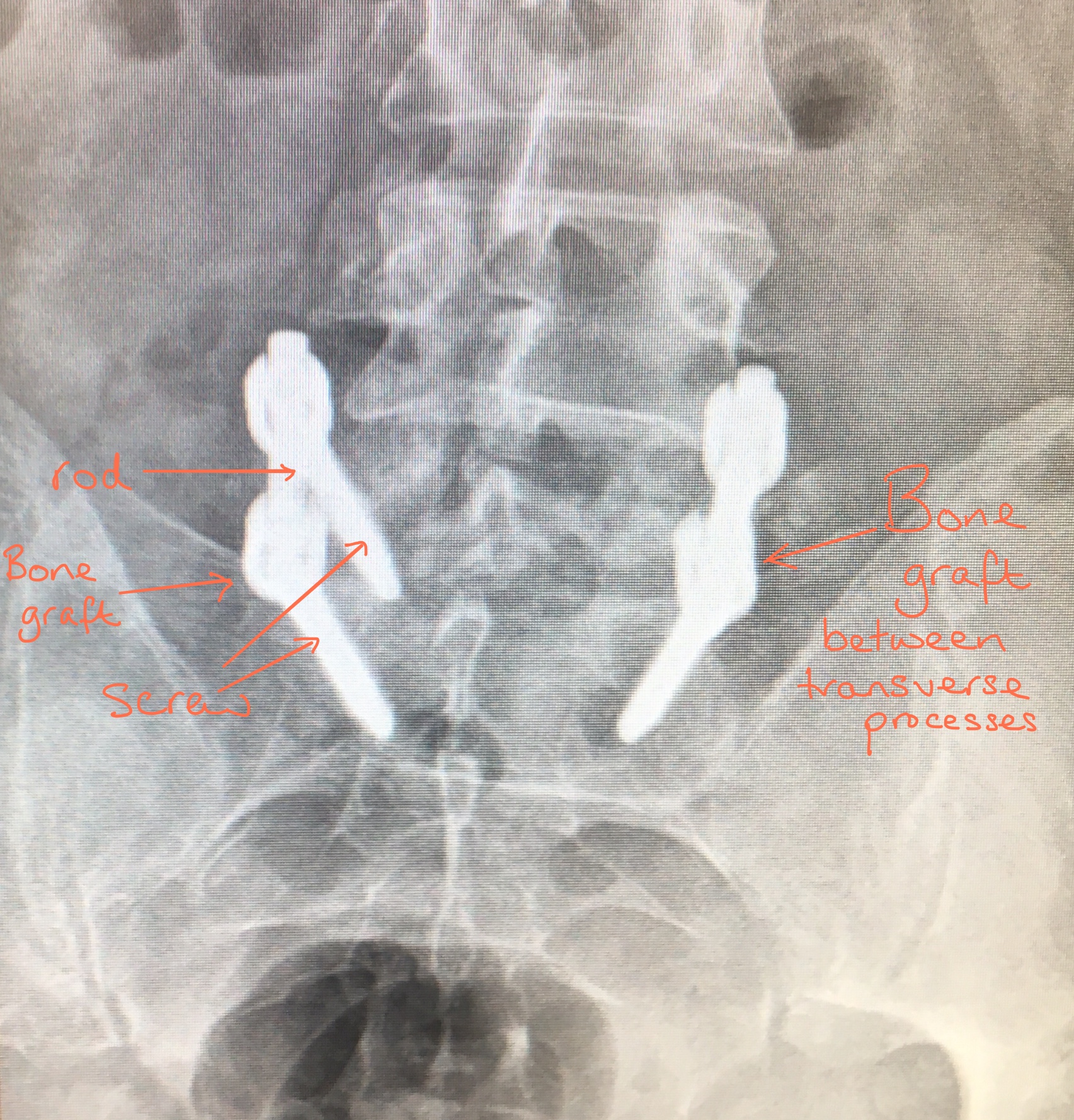
The above X-ray demonstrates a posterior-lateral fusion; where the screws, rods and bone graft is placed. Note there is no interbody cage.
Risks And Complications Of Posterior Lumbar Instrumented Fusion
- Bleeding including minor and major vascular damage which can be life-threatening (1 in 10,000 patients)
- Superficial infection: 4 in 100 patients
- Deep infection: 1 in 100 patients.
- DVT/Pulmonary embolism
- Bruising and swelling around the surgical site
- Wound dehiscence (wound opens up and requires closing again)
- Minor and major nerve damage (including foot drop, cauda equina syndrome, paralysis) which can be temporary or permanent – more common in revision surgery.
- Dural tear (CSF leak): 5 in 100 patients with a higher risk in revision surgery
- Return to theatre to re-repair a dural tear: 0.05% of patients
- Recurrent leg pain due to perineural fibrosis (scarring around nerves)
- Damage to surrounding soft tissues including muscle
- Failure of Bone Fusion: 5 in 100 patients
- Difficulty with screw placement leading to nerve injury
- Failure of implants and misplacement of Implants (screws, cages, plate)
- Cage (implant) movement: 2 in 100 patients, with 1 in a 100 patients requiring re-operation.
- Failure to relieve symptoms or recurrence of symptoms: 70% of patients will gain 50% improvement
- Worse pain/symptoms
- Back pain
- Medical Complications including stroke (CVA), heart attack (MI), blindness and death
Mr Hilton will take time to thoroughly go through all the risks and complications of a sacro-iliac joint fusion before you decide whether to proceed with the surgery. The risks and complications are similar to those of all spinal surgeries however in fusion surgery, the surgery time is longer and the nerves are retracted/protected for longer and consequentially this carries more risk of complications.
More detailed information about the general risks and complications please look at the ‘Risks and Complications’ section.
Factors which may affect spinal fusion and your recovery
There are a number of factors that can significantly reduce the chances of a solid fusion following surgery and these include:
• smoking
• diabetes or chronic illnesses
• obesity
• malnutrition
• osteoporosis
• post-surgery activities (twisting exercises, lifting heavy weights, not taking medical advice on what activities you should be doing)
• long-term (chronic) steroid use
Of all these factors, smoking has the biggest negative effect on bone fusion (and the risk of post-operative infections). Nicotine is a bone toxin (poison) and can inhibit the ability of the bone-growing cells in the body (osteoblasts) to grow bone and therefore stop the bone fusion. In order to give yourself the best chance of bone fusion, you should stop smoking ideally 2 -3 months before your surgery.
Your surgery may be delayed if you have not stopped smoking (or taking nicotine in another form) beforehand.
There is evidence that NSAIDs (Non-steroidal anti-inflammatory drugs) including ibuprofen, naproxen, diclofenac, meloxicam and aspirin may slow or even prevent bone fusion.
NSAIDs affect prostaglandin synthesis, and, as prostaglandins are essential for normal bone turnover and new bone formation, the use of NSAIDS may ultimately affect bone healing by inhibiting new bone formation. Animal studies involving NSAIDs have shown a delay in healing time and non-union but no long term studies have been done on humans yet. Although it is a theoretical risk, a lot of spinal surgeons worldwide advise patients not to take NSAIDs following spinal fusions.
If you need to take NSAIDs, for example for rheumatoid arthritis or osteoarthritis, please discuss this with Mr Hilton.
BMI > 35
Having a high BMI (Body Mass Index) has a negative impact on bone fusion following a spinal fusion.
Furthermore, if your BMI is greater than 35 it is highly unlikely than you will be considered for a spinal fusion for anaesthetic reasons.
Recovery
Following surgery, most patients usually stay in hospital for 2-3 days and this partly depends on their general health. In order to allow the fusion to heal and to allow patients to mobilise adequately, some patients are discharged home on crutches. Some pain/tenderness and bruising is normal around the operation site and usually patients feel this is different in nature to the back pain they were experirncing before the operation.
Prior to your discharge, you will spend time with the hospital physiotherapist who will help you to mobilise (with crutches if needed) and they will advise you on appropriate exercises to do once you return home. It is essential you practice these exercises everyday.
Mr Hilton or one of his team will see you at about 7 – 10 days following your operation to check your wound and also to see how you are getting on. All patients are advised NOT to change their dressings. You are at risk of getting a wound infection if you change your own dressing.
If you are concerned about your wound or you feel it is necessary to change the dressing before your wound check appointment, then either:
Place a fresh dressing over the top of the original dressing
OR
Contact the hospital or your GP practice.
Physiotherapy
The first part of your treatment is stabilising the spine and taking the pressure off the spinal nerves, the second part of your treatment journey is your rehabilitation which involves exercise. You will be referred to a physiotherapist as an outpatient, however before you see the physiotherapist please continue to do the exercises you were taught in hospital on a daily basis.
The aim of doing exercises is to rehabilitate and improve the strength of the muscles supporting the spine and pelvis.