Sacro-iliac joint dysfunction is a very painful and sometimes debilitating condition that limits patient’s activity levels and affects their day to day functioning.
If all conservative treatments have failed and you have had two positive, diagnostic sacro-iliac joint injections then you may want to consider a sacro-iliac joint fusion.
The Surgical Procedure
Mr Hilton uses a minimally invasive (keyhole) surgical procedure to perform a sacro-iliac joint fusion as opposed to open surgery. In particular he uses a system called the iFuse Implant System which typically uses three titanium iFuse implants (see second diagram to the right). He has been specially trained to use this technique and favours it because both the surgical technique and the implant are designed to protect the tissues (eg muscles, nerves) surrounding the surgical site.
The operation is done under general anaesthetic and therefore you need to be fit and well enough to have a general anaesthetic. You will be assessed by Mr Hilton’s anaesthetist before the operation.
During the operation a small incision is made, usually 3 – 5cm long over the side of the hip/buttock. During the operation, a special X-ray imaging technique called fluoroscopy is used which provides real-time images of the internal structures during the operation. Special surgical instruments are used to prepare the bone and help place the titanium implants across the sacro-iliac joint.
The operation takes about one hour however you will be in operating suite for longer both before and after the operation due to the anaesthetic. Typically you will spend 1 -2 days in hospital following the operation and will be seen 7- 10 days later for a wound check appointment and to see how you are doing.
NICE (the UK’s National Institute for Clinical Excellence) latest guidance states:
“NICE develops guidance and quality standards in health and social care and is a worldwide leader in technology evaluations. NICE’s role is to improve outcomes for people using the NHS and other public health services.
The recommendation states that the safety and efficacy of minimally invasive sacroiliac joint fusion surgery is adequate provided that standard arrangements are in place. They also recommend that the procedure be performed by trained surgeons using a lateral transarticular approach, and that patients have been properly diagnosed with sacroiliac joint dysfunction due to degenerative sacroiliitis or sacroiliac joint disruption.”
Outcomes:
Evidence shows that almost 70% of patients had a reduction in the sacro-iliac joint pain following surgery with iFuse implant system and 88% would have the operation again.

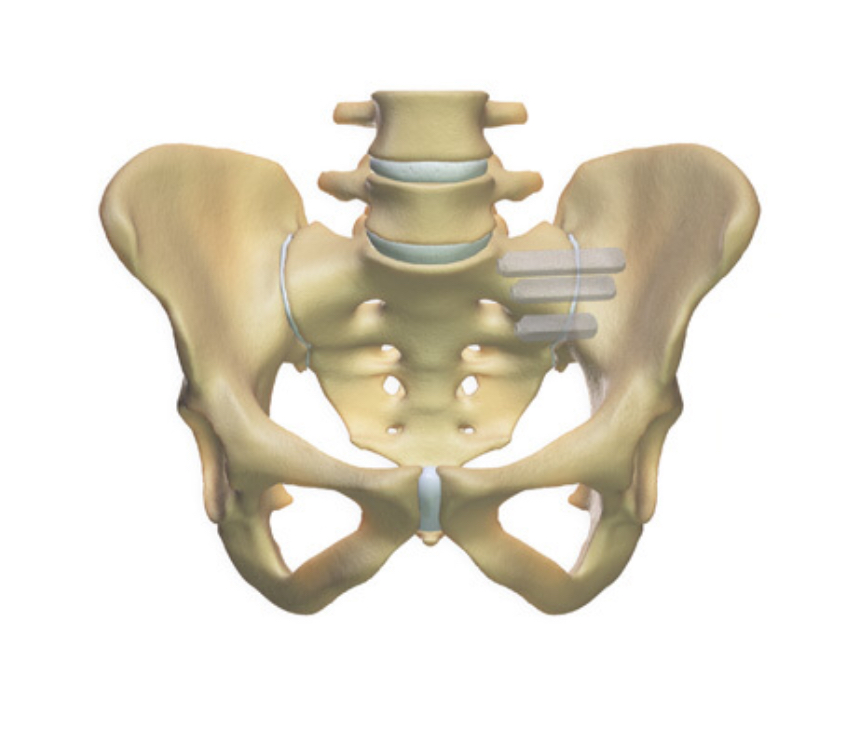
The 3-D image above demonstrates where the three implants are placed across the sacro-iliac joint to achieve the fusion.
X-rays of a Sacro-iliac Joint Fusion

X-ray showing the position of the implants from the front

X-ray shows implants looking from a side view
Risks And Complications Of Sacro-Iliac Joint Fusion
- Bleeding (minor and major vascular damage which can be life-threatening)
- Bruising and swelling around the surgical site
- Infection
- DVT/Pulmonary Embolism
- Wound dehiscence
- Minor and Major Nerve Damage (including foot drop, cauda equina syndrome, paralysis) which can be temporary or permanent
- Damage to surrounding soft tissues including muscle
- Failure of Bone Fusion
- Perineural Fibrosis
- Failure to Relieve symptoms or Recurrence of Symptoms
- Failure of Implants and Misplacement of Implants
- Medical Complications (including CVA, MI, Blindness and Death)
Mr Hilton will take time to thoroughly go through all the risks and complications of a sacro-iliac joint fusion before you decide whether to proceed with the surgery. The risks and complications are similar to those of spinal surgery and therefore for more detailed information about the general risks and complications please look at the ‘Risks and Complications’ section. For more information about the risks and complications specific to sacro-iliac joint fusion, please look on the SI-BONE website.
Factors Which May Affect Spinal Fusion And Your Recovery
There are a number of factors that can significantly reduce the chances of a solid fusion following surgery and these include:
• smoking
• diabetes or chronic illnesses
• obesity
• malnutrition
• osteoporosis
• post-surgery activities (twisting exercises, lifting heavy weights, not taking medical advice on what activities you should be doing)
• long-term (chronic) steroid use
Of all these factors, smoking has the biggest negative effect on bone fusion (and the risk of post-operative infections). Nicotine is a bone toxin (poison) and can inhibit the ability of the bone-growing cells in the body (osteoblasts) to grow bone and therefore stop the bone fusion. In order to give yourself the best chance of bone fusion, you should stop smoking ideally 2 -3 months before your surgery.
Your surgery may be delayed if you have not stopped smoking (or taking nicotine in another form) beforehand.
There is evidence that NSAIDs (Non-steroidal anti-inflammatory drugs) including ibuprofen, naproxen, diclofenac, meloxicam and aspirin may slow or even prevent bone fusion.
NSAIDs affect prostaglandin synthesis, and, as prostaglandins are essential for normal bone turnover and new bone formation, the use of NSAIDS may ultimately affect bone healing by inhibiting new bone formation. Animal studies involving NSAIDs have shown a delay in healing time and non-union but no long term studies have been done on humans yet. Although it is a theoretical risk, a lot of spinal surgeons worldwide advise patients not to take NSAIDs following spinal fusions.
If you need to take NSAIDs, for example for rheumatoid arthritis or osteoarthritis, please discuss this with Mr Hilton.
Recovery
Following surgery, most patients usually stay in hospital for 1-2 days and this partly depends on their general health. In order to allow the SI joint to heal properly, patients can only partially weight-bear on the side of the operation for 2-3 weeks and therefore will be discharged on crutches (even if you do not feel like you need them). It may help to apply an ice pack over the wound (although the dressing MUST NOT be removed) to help reduce the swelling. Some pain/tenderness and bruising is normal around the operation site.
Prior to your discharge, you will spend time with the hospital physiotherapist who will help you learn to walk with crutches so that you are partially weight-bearing. In addition the physiotherapist will advise you on appropriate exercises to do once you return home. It is essential you practice these exercises everyday.
What is partially weight-bearing?
Partially weight-bearing means putting only 20% of your weight through your operated leg. This can be difficult to imagine, so using a set of weighing scales, place your foot on the scales and apply pressure until you achieve 20% of your body weight – for example, 2 stone if you weigh 10 stone or 13kg if you 65kg.
Mr Hilton or one of his team will see you at about 7 – 10 days following your operation to check your wound and also to see how you are getting on. Patients are advised NOT to change their dressings. You are at risk of getting a wound infection if you change your own dressing.
If you are concerned about your wound or you feel it is necessary to change the dressing before your wound check appointment, then either:
Place a fresh dressing over the top of the original dressing
OR
Contact the hospital or your GP practice.
Physiotherapy
The first part of your treatment is stabilising and fusing the SI joint, the second part of your treatment journey is your rehabilitation which involves exercise. You will be referred to a physiotherapist as an outpatient, however before you see the physiotherapist please continue to do the exercises you were taught in hospital on a daily basis.
The aim of doing exercises is to rehabilitate and improve the strength of the muscles supporting the pelvis and SI joint.