What is Sciatica?
The definition of sciatica is pain that runs down the entire length of the sciatic nerve (the longest nerve in the body) – the pain spreads from the buttocks down the back of the thigh and calf and into the foot.
It is usually caused by a disc prolapse (also called a bulge or herniation) or spinal stenosis.
What is the difference between Sciatic nerve pain and other radicular leg pain?
The sciatic nerve is formed from the L4, L5, S1, S2 and S3 nerves joining together and forming a single nerve – the longest nerve in the body. This is why sciatica usually travels down the whole leg into the foot.
Sciatica refers to pain NOT numbness, altered or loss of sensation.
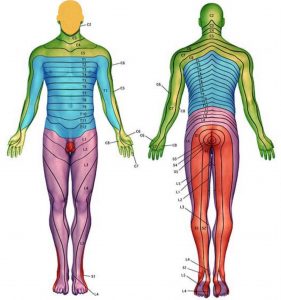
Different lumbar nerve roots map out different areas on the leg and therefore pain is felt in these specific areas if these nerves are irritated; this is called ‘radicular’ leg pain. For example, pain caused by irritation of the L2 nerve root typically causes pain to radiate into the groin and across the top of the thigh to the inside of the thigh; this would be called ‘L2 radicular pain’. This pain can be very similar to the pain that is caused by pain coming from the hip joint so the history and examination are very important.
Furthermore, when looking at the MRI scan there may be disc prolapses or stenosis at other levels in the spine but initially the focus would be, for example, on the L2 nerve root as this is where the problem is. As a general rule, if considering surgery, only the level causing a problem are operated on because operating on any other levels that are not causing a problem just increases the risk of something going wrong.
See the map of the dermatomes which illustrates where irritation of the different nerves are usually felt.

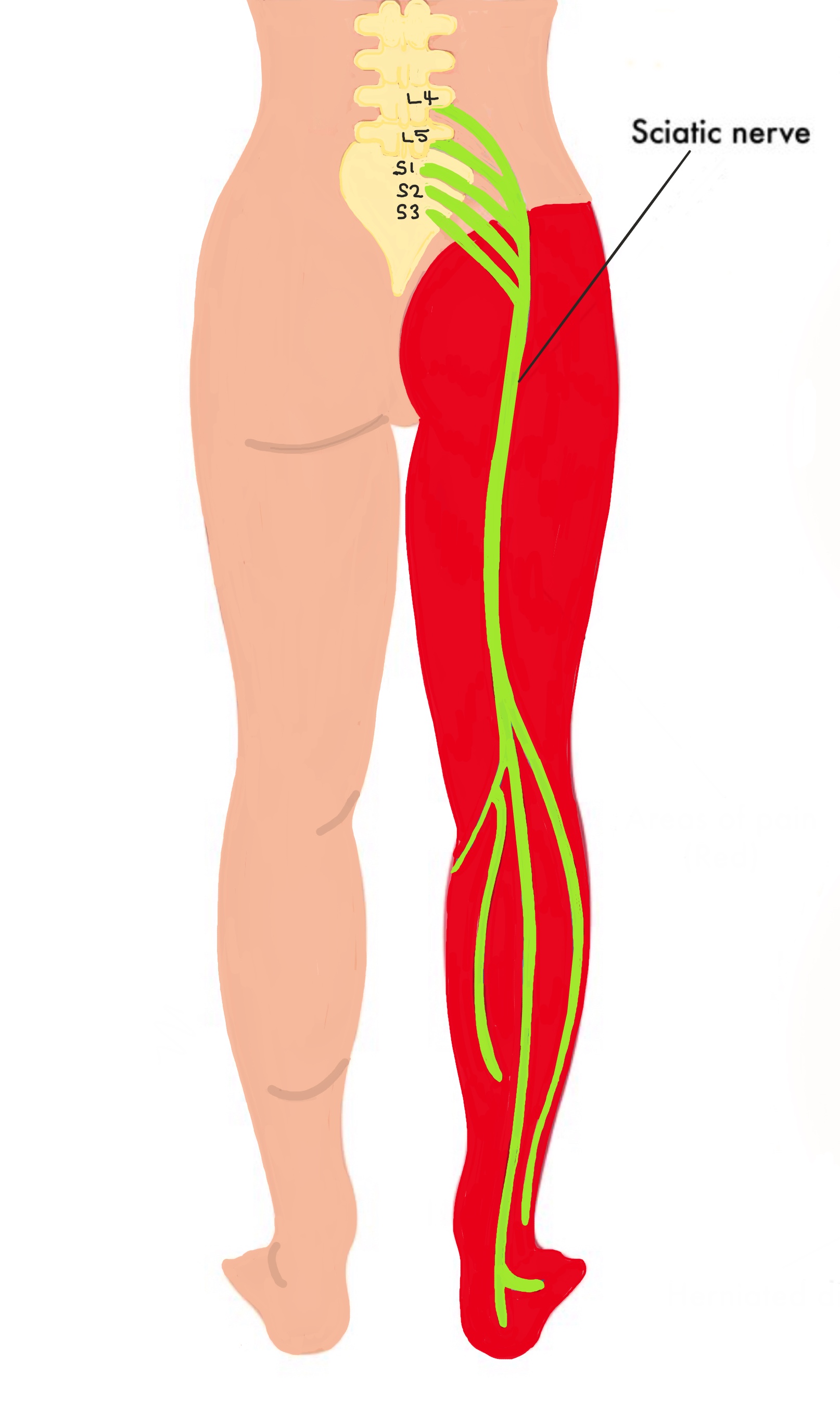
The diagram shows the sciatic nerve and the red area shows the distribution of pain caused by sciatica.
What is the difference between pain, numbness, reduced sensation, altered sensation, burning sensation, pins and needles?
Lumbar spinal nerves carry messages from the legs to the brain about sensation. They also carry messages to the muscles in the legs to make them move and function. Some of these nerves also control the bladder, bowels and sexual function.
When nerves get pressed on or irritated, they send warning messages to the brain in the form of pain, burning sensation, reduced or altered sensation. Sometimes the irritation of the nerve causes weakness in a certain muscle group (called a ‘myotome’) that is supplied by that nerve.
‘Numbness’ means the nerve is dead and if you were to put a needle into your leg you would not feel it – if you can feel a needle being stuck into you then your sensation is reduced and is not described as ‘numbness’. Although reduced and altered sensation maybe very annoying, and sometimes debilitating, it is not the same as pain – it is important to distinguish between pain and reduced or altered sensation.
‘Radicular pain’ is a term doctors use to describe pain originating from a specific nerve root. Leg pain may also be referred from the back, however generally the leg pain does not go below the knee and is improved by treating the underlying back pain.
The size of the disc prolapse is NOT always proportional to the amount of pain or weakness felt. A very small disc prolapse in the wrong place can cause severe pain whereas a large, central prolapsed disc may not cause any symptoms.
What treatment is available?
Treatment options then depend upon the severity and duration of the symptoms as well as the underlying cause. Changes seen include facet joint arthritis, degenerative disc disease and spondylolisthesis. Treatment options then fall into three main categories.
Physical therapy
Improving spinal mobility, core muscle strength and overall fitness may improve the pain to a manageable level.
The natural history of the condition is that over 90% of patients will improve with no interventional treatment. Simple pain control, using over the counter medication such as paracetamol or anti-inflammatories, eg. Ibuprofen, are helpful. Occasionally, diazepam can be used to help relieve back spasm and break the pain cycle and help improve mobility but this should be discussed with your GP and should only be used for a few days.
Spinal Injections
X-ray guided epidurals and nerve root blocks can be extremely useful in patients to help to relieve leg pain (and sometimes altered sensation) associated with a disc prolapse, while the natural healing occurs. They are also very useful in the diagnostic process and they can confirm or exclude a diagnosis. Spinal injections have the advantage of being performed under local aneasthetic or sedation and although there are potential risks and side effects, these are extremely rare. Also it is estimated that 60% of patients will have significant relief of symptoms, which may be permanent. See section on spinal injections for more information.
Surgery
Surgery, in the form of a lumbar microdiscectomy, may be considered under the following circumstances:
- Central disc prolapse pressing on the nerves to the bladder or bowel (cauda equina syndrome)
- Progressive weakness within the leg
- Severe pain not responding to conservative measures within the first 6 weeks of onset
- Persistent pain affect activities at 6 weeks or more following surgery