Intervertebral disc prolapses are very common and they do not always cause problems. Disc prolapses are also called ‘herniated’, ‘slipped’, ‘bulging’ or ‘ruptured’ discs.
It is estimated that about 55% of the population aged over 60 years old and about 20% of people under 60 have at least one prolapsed disc – however of these people, about 15% of those under 40 years are pain-free and have no symptoms and this is increased to almost 30% in people over 40 years old.
So the important thing to remember is, just because you have a disc prolapse does not mean you will have symptoms and it certainly does not necessarily mean you need surgery.
The most common disc prolapses in the lower lumbar spine are at the L4/5 and L5/S1 levels between the ages of 25-55 years and above these levels in the over 55 age group.
What is an intervertebral disc and how does it herniate?
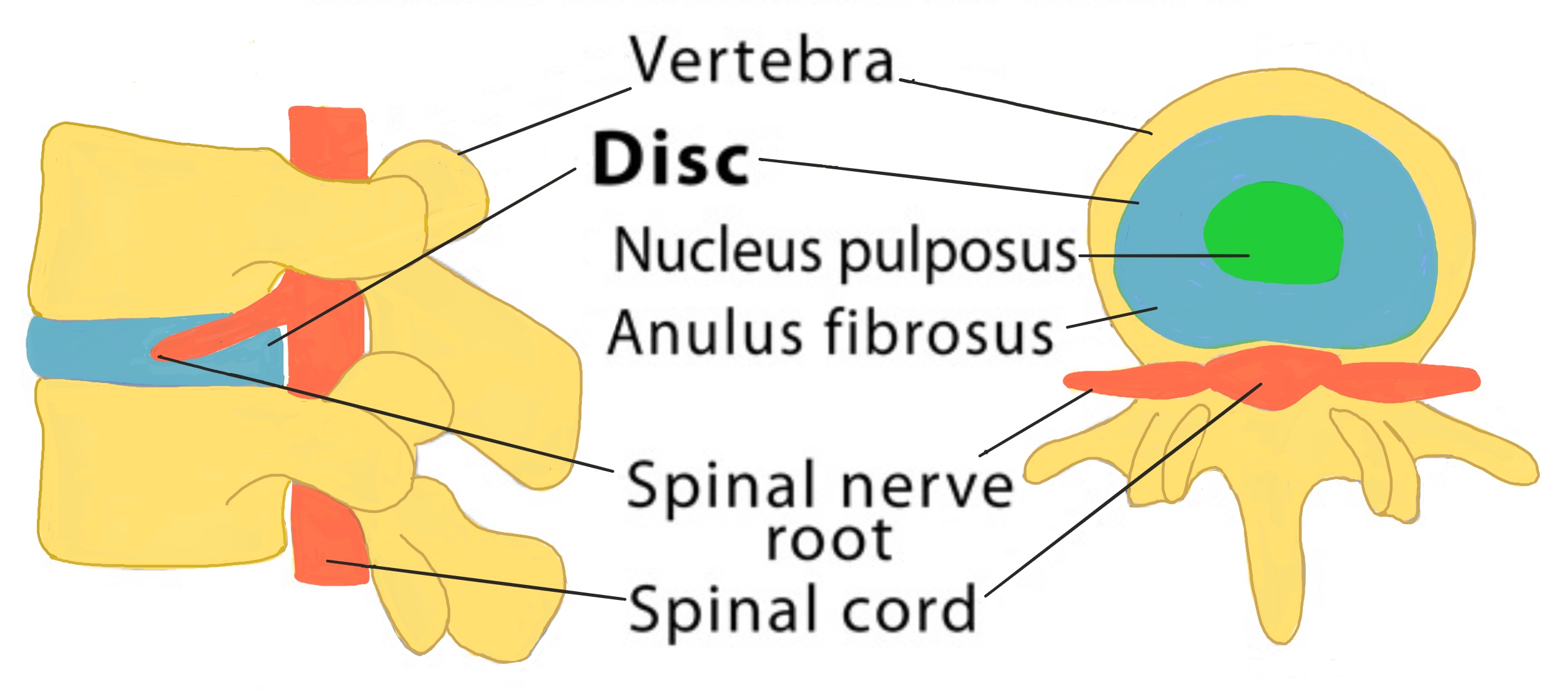
Between each of the vertebral bones is an intervertebral disc and they account for a quarter of the entire length of the spine (which is why people get shorter as they get older as the discs start to degenerate). Discs are found above and below each vertebral bone except between the first and second cervical vertebrae (C1 and C2) and also between the coccygeal vertebrae. Discs act like a cushion between the bones and work as shock absorbers to protect the vertebrae, brain, spinal cord and spinal nerves. The discs also allow some limited movement between the vertebrae to allow us to be flexible.
Intervertebral discs are a similar shape to a jam doughnut. Each disc contains a tough, fibrous outer layer called the annulus fibrosus that surrounds a soft, gel-like middle part called the nucleus pulposus (the jam part of the doughnut). The discs are made of a fibrocartilaginous material that have no blood supply themselves so rely on the vertebrae above and below for nutrients. However they do have a nerve supply.
When healthy, the discs are able to attract and retain water so they can effectively act as shock absorbers. The gel-filled nucleus attracts and holds the most water although this amount varies throughout the day depending on activity.
Some people are more genetically pre-disposed to getting disc problems than others, however these are the main reasons for discs to herniate or prolapse:
- ‘Degeneration’: As we get older and, with everyday wear and tear, the discs start to ‘degenerate’. The outer layer starts to get weaker and the gel-like middle layer breaks through it or in order words “herniates”.
- ‘Trauma’: Sudden, abnormal pressure or load on the disc can cause the soft, gel-like middle to herniate through the fibrous wall of the disc. – imagine squashing a jam donut too much and the jam squirting out. Trauma includes lifting something too heavy, and especially if twisting at the same time, or a car accident.
- ‘Trauma and Degeneration’: In discs that are already weakened by degeneration, only a small amount of pressure or trauma is required to cause the nucleus pulposus to herniate, for example lifting the washing out of the washing machine or even just sneezing.

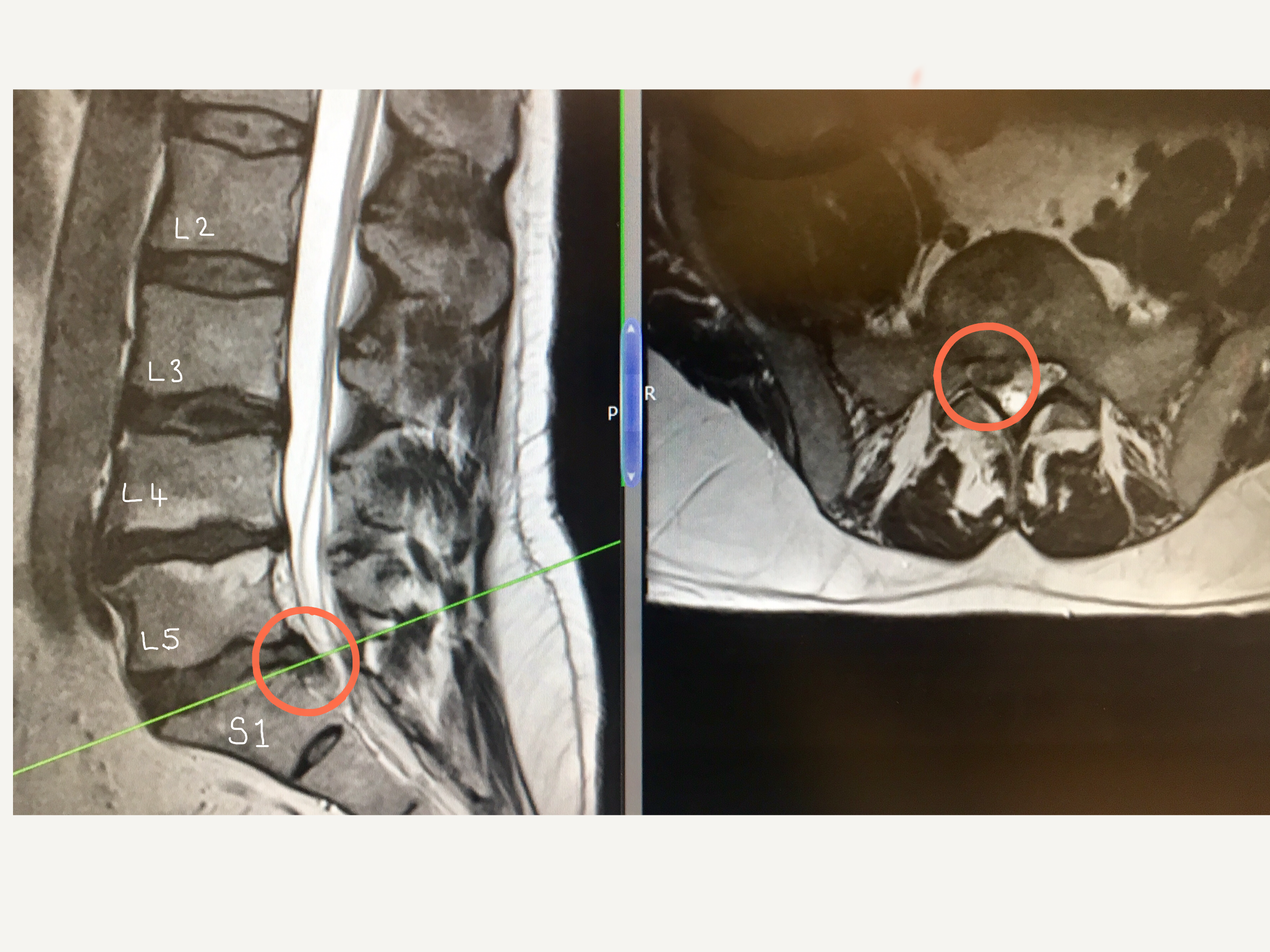
The circled areas on the MRI scan images show a disc bulge at the L5/S1 level. The image on the left is a view of the spine looking from the side (lateral view) and the image on the right shows the corresponding cross-section (axial view). The herniated disc in this image is pressing on the L5 spinal nerve root.

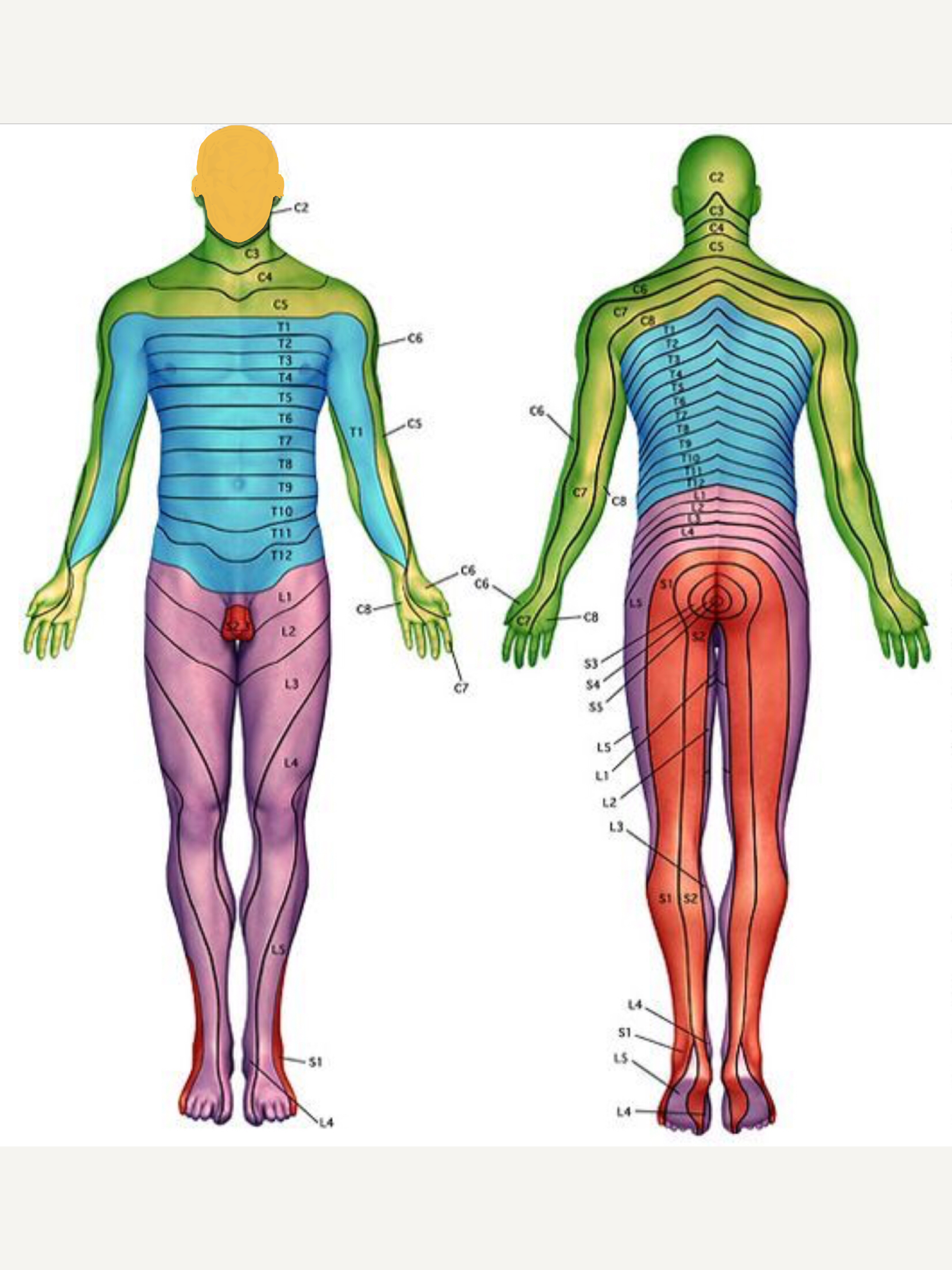
The dermatome chart above illustrates where symtoms are felt on the body in relation to the different nerve roots.
Symptoms
As previously mentioned, not all prolapsed disc cause symptoms. However, for those people who do experience symptoms, where the symptoms are felt depends on what level the disc has herniated at. Different nerve roots in the spine supply different areas of the body. The different lumbar nerve roots correspond to different patterns of symptoms in the legs depending on their level. For example, if the L5 nerve root is being pressed on then the person typically feels symptoms in the buttock, side of the thigh and calf, wrapping around to the front of the ankle onto the top of the foot and big toes. Whereas if a the L3 nerve is being pressed on then most of the pain is felt in the front and inside if the thigh. This is shown in the pictorial form in the ‘Dermatome Chart’ on he left.
Symptoms of a lumbar disc prolapse can be in one leg or both legs and include:
- Pain
- Burning sensation
- Loss or reduced sensation including numbness
- Altered sensation including tingling, pins and needles, sensations of water running down the leg
- Weakness or loss of power
- Low back pain
- Loss of bowel, bladder or sexual sensation/function – this is rare and is called cauda equina syndrome and you should seek urgent medical attention.
Most symptoms following a disc prolapse or herniation will resolve naturally between 6 -1 2 weeks without any treatment. It is best to keep as active as possible and take painkillers. If the pain is severe then a guided steroid epidural or nerve root injection can help to accelerate the resolution of symptoms. Although the disc prolapse/herniation is unlikely to disappear, it may shrink but most importantly the symptoms may have resolved. If the symtoms do not resolve after 12 weeks a referral to a spinal surgeon maybe be needed.
Diagnosis
Mr Hilton always takes a detailed history and performs a neurological examination as the first of any diagnosis process. Imaging is used usually to confirm, or exclude, a diagnosis and this is generally in the form of standing X-rays, a MRI and occasionally a CT scan .
The important thing to remember is that although you may have a wear and tear or a prolapsed disc, the symptoms need to match your scan. For example, a disc prolapse at L5/S1 does not usually cause pain down the front of your thigh as that is more likely to be coming from the L2/3 level.
What treatment is available?
Treatment options then depend upon the severity and duration of the symptoms as well as the underlying cause. Changes seen include facet joint arthritis, degenerative disc disease and spondylolisthesis. Treatment options then fall into three main categories.
Physical therapy
Improving spinal mobility, core muscle strength and overall fitness may improve the pain to a manageable level.
The natural history of the condition is that over 90% of patients will improve with no interventional treatment. Simple pain control, using over the counter medication such as paracetamol or anti-inflammatories, eg. Ibuprofen, are helpful. Occasionally, diazepam can be used to help relieve back spasm and break the pain cycle and help improve mobility but this should be discussed with your GP and should only be used for a few days.
Spinal Injections
X-ray guided epidurals and nerve root injections can be extremely useful in patients to help to relieve leg pain (and sometimes altered sensation) associated with a disc prolapse, while the natural healing occurs. They are also very useful in the diagnostic process and they can confirm or exclude a diagnosis. Spinal injections have the advantage of being performed under local aneasthetic or sedation and although there are potential risks and side effects, these are extremely rare. Also it is estimated that 60% of patients will have significant relief of symptoms, which may be permanent.
Surgery
Surgery, in the form of a lumbar discectomy, may be indicated under the following circumstances:
- Central disc prolapse pressing on the nerves to the bladder or bowel (cauda equina syndrome)
- Progressive weakness within the leg
- Persisting, severe pain not responding to conservative measures

Recovery
Will I get better?
In most patients the symptoms improve within six weeks with physiotherapy treatment and analgesics. Occasionally the pain does not better or there is weakness in the legs and then surgery may be considered.
What will the long-term effects of a disc prolapse be?
Unfortunately following the disc prolapse, the disc will always be abnormal but that not mean you will always have symtoms. A percentage of patients will experience back pain as a result of the disc prolapse, irrespective of whether surgery is performed or not.
Will the disc prolapse come back?
About 10% of patients will have a recurrent disc prolapse – this means some more of the nucleus pulposus (the middle soft gel-like part of the disc) herniates through the annulus fibrosis (the tough outer wall) and irritates a nerve to cause leg pain. The risk of this is greatest immediately following the operation and decreases with time. Also, unfortunately, some people are genetically predisposed to disc prolapses and have other close family members with the similar problems.