Intervertebral disc prolapses are very common and they do not always cause problems. Disc prolapses are also called ‘herniated’, ‘slipped’, ‘bulging’ or ‘ruptured’ discs.
The gel-like middle part of the lumbar disc (nucleus pulposis) bulges through the surrounding, tough fibrous tissue (annulus fibrosis) and may cause irritation or compression of an adjacent nerve. This often occurs in the presence of an abnormal or degenerate disc, which has a small tear in the annulus fibrosis. The disc prolapse can cause nerve compression and irritation.
When nerves get pressed on or irritated, they send warnings messages to the brain in the form of pain, burning sensation, reduced or altered sensation. Sometimes the irritation of the nerve causes weakness in a certain muscle group (called a ‘myotome’) that is supplied by that nerve.
Symptoms of a lumbar disc prolapse.
Not all prolapsed discs cause symptoms. However, for those people who do experience symptoms, where the symptoms are felt depends on what level the disc has herniated at. Different nerve roots in the spine supply different areas of the body. The different lumbar nerve roots correspond to different patterns of symptoms in the legs depending on their level. Often prolapsed discs do not cause back pain.
Most Symptoms of a lumbar disc prolapse can be in one leg or both legs and include:
- Pain
- Burning sensation
- Loss or reduced sensation including numbness
- Altered sensation including tingling, pins and needles, sensations of water running down the leg
- Weakness or loss of power
- Low back pain
- Loss of bowel, bladder or sexual sensation/function – this is rare and is called Cauda Equina Syndrome and you should seek urgent medical attention.
Most symptoms following a disc prolapse or herniation will resolve naturally between 6 -1 2 weeks without any treatment. It is best to keep as active as possible and take painkillers. If the pain is severe then a guided steroid epidural or nerve root injection can help to accelerate the resolution of symptoms.
If the pain does not resolve after 12 weeks or after a steroid injection, or if there is weakness, spinal surgery may be considered. If there are symptoms of Cauda Equina Syndrome, urgent surgery is indicated.

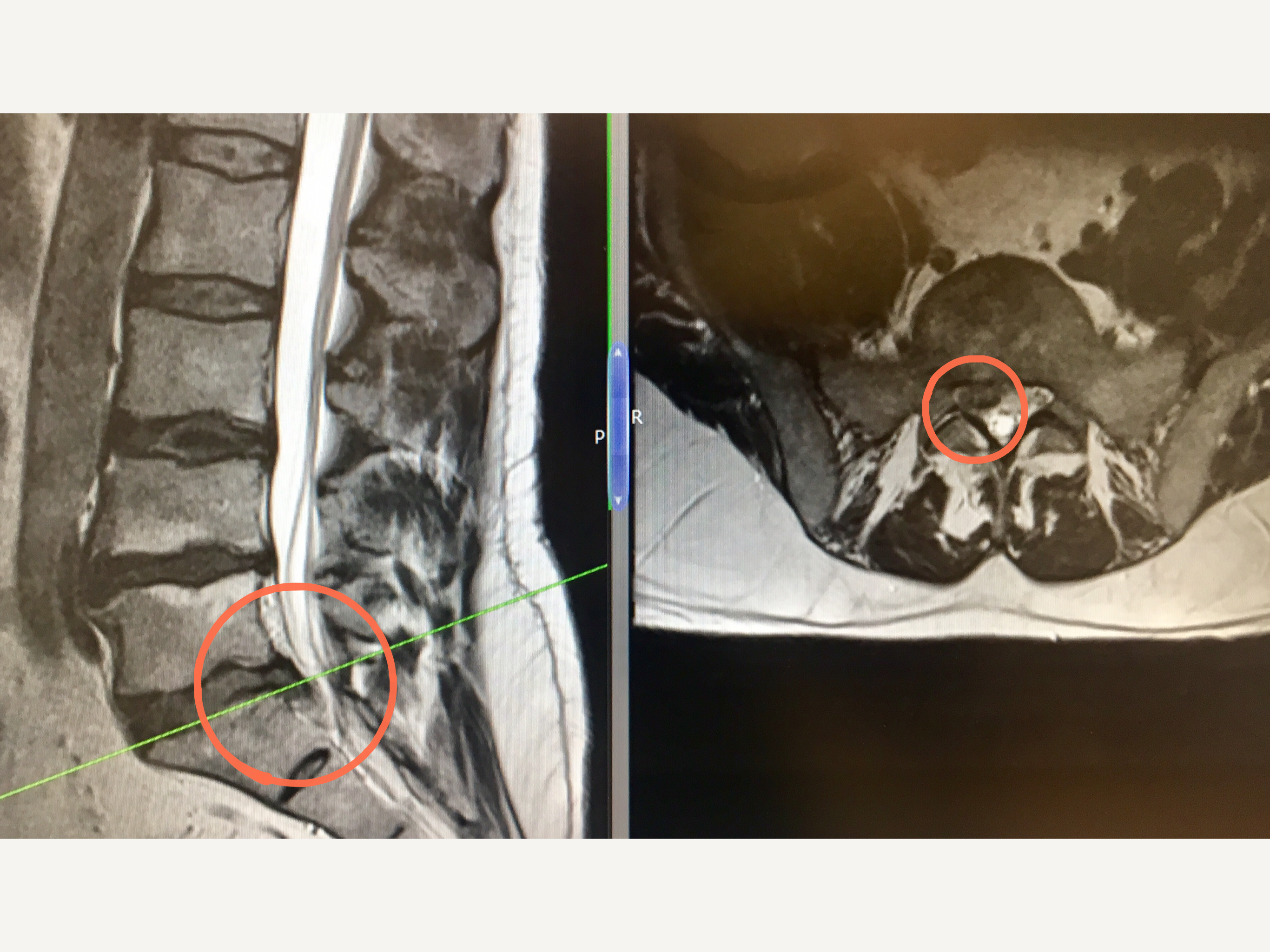
The MRI images show a large right-sided disc bulge at L5/S1 before the microdiscectomy operation.
Lumbar Microdiscectomy
All lumbar microdiscectomies are performed in theatre under a general anaesthetic and typically most patients stay in hospital for 1 – 2 days.
Mr Hilton performs all discectomies and decompression under X-ray guidance (to confirm the correct level) and with the use of a surgical microscope – this allows an excellent, magnified view of the whole of surgical area. In a (micro)discectomy only the protruding/bulging part of the disc is removed, not the whole disc.
The whole operation is performed through a small incision which is about 3cm long, however it maybe longer especially if the operation involves more than one level.
The first part of the operation is gaining access to the spinal canal which involves removing a small amount of bone and ligament. The irritated nerve root lies on top of the disc that is being operated on, therefore the nerve has to be carefully moved and protected (‘retracted’) for the next part of the operation.
Often nerves that have been compressed or irritated can be ‘stuck’ down onto the disc and so it can be quite difficult to simply move the nerve out of the way. Once the nerve is moved out of the way and protected, the prolapsed disc material is removed as is any other tissue that is causing increased pressure on the nerve.
Results:
70 – 80% of people who have a Microdiscectomy describe a significant improvement in their leg pain.
Risks And Complications of Microdiscectomy
- Bleeding (minor and major vascular damage which can be life-threatening)
- Bruising around the surgical site
- Infection
- DVT/Pulmonary Embolism
- Dural tear/CSF leak (3% risk in a primary microdiscectomy)
- Minor and major nerve damage (including foot drop, cauda equina syndrome, paralysis) which can be temporary or permanent
- Damage to surrounding soft tissues including muscle
- Perineural fibrosis (scarring around nerves causing a recurrence of pain)
- Wound dehiscence
- Failure to relieve symptoms, recurrence of symptoms
- Worse symptoms
- Back pain
- Medical Complications including stroke (CVA), heart attack (MI), blindness and death
Mr Hilton will take time to thoroughly go through all the risks and complications of a microdiscectomy before you decide whether to proceed with the surgery.
More detailed information about the general risks and complications please look at the ‘Risks and Complications’ section.
Recovery
Everybody is different! Initially when pressure is taken off a nerve some patients immediately feel pain relief whereas for others it can take a few days. This is because nerves that are inflamed take time to settle and surgery itself can cause some temporary inflammation of nerves.
The main aim of a Microdiscectomy is to take the pressure off the nerve and to stop pain and prevent any further loss of power. It is very difficult to predict whether altered sensation or numbness will improve and unfortunately for some it does not improve despite a good operation.
After surgery it is not uncommon to have various aches and pains in and around the wound, and in the bony pelvis, hips and thighs. These usually improve with time.
Following surgery, most patients usually stay in hospital for 1 – 2 days and this partly depends on their general health. Some pain/tenderness and bruising is normal around the operation site and usually patients feel this is different in nature to the back pain they were experiencing before the operation.
Prior to your discharge, you will spend time with the hospital physiotherapist who will help you to mobilise (with crutches if needed) and they will advise you on appropriate exercises to do once you return home. It is essential you practice these exercises everyday.
Mr Hilton or one of his team will see you at about 7 – 10 days following your operation to check your wound and also to see how you are getting on. All patients are advised NOT to change their dressings. You are at risk of getting a wound infection if you change your own dressing.
If you are concerned about your wound or you feel it is necessary to change the dressing before your wound check appointment, then either:
Place a fresh dressing over the top of the original dressing
OR
Contact the hospital or your GP practice.
Depending on your job, most patients are able to return to work 6 weeks after the surgery.
Physiotherapy
The first part of your treatment is to take the pressure off the affected spinal nerve, the second part of your treatment journey is your rehabilitation which involves exercise. You will be referred to a physiotherapist as an outpatient, however before you see the physiotherapist please continue to do the exercises you were taught in hospital on a daily basis.
The aim of doing exercises is to rehabilitate and improve the strength of the muscles supporting the spine and pelvis.