‘Stenosis’ originates from a Greek word that means ‘narrowing’ and therefore ‘spinal stenosis’ means ‘narrowing of the spinal canal’.
Spinal stenosis is common and can happen anywhere in the spine but usually occurs in the lumbar spine (low back) and the cervical spine (the neck) because these are the most mobile parts of the spine and therefore most prone to wear and tear. Narrowing of the spinal canal can result in abnormal pressure on the spinal cord and spinal nerves, however not everyone who has spinal stenosis has symptoms.
Spinal stenosis is most common in the older people however it can occur in young people.
What causes spinal stenosis?
Each bone (vertebra) in the spine has a hole or space in the middle of its body. The bones fit together forming a hollow ‘canal’ that encases and protects the soft spinal cord and spinal nerves.
People are born with different size canals just as they are born with different size feet. Some people are born with a congenitally small canals (also called ‘congenital spinal stenosis’) and they are at more risk of developing spinal stenosis than other people. Likewise, those who are born with a larger canals are less likely to develop significant spinal stenosis.
The main causes of spinal stenosis are:
1. Degenerative or “Wear and Tear”
Spinal stenosis due to wear and tear is the most common cause and is part of the natural ageing process. The wear and tear affects three different parts of the spine thereby creating a three-pronged attack on the spinal cord and nerves:
- Degenerative discs: In combination with getting older and with everyday wear and tear, the intervertebral discs start to degenerate and lose their shape. The outer layer starts to get weaker and bulges into the spinal canal.
- Osteoarthritis (‘wear and tear’) of the facet joints results in bony spurs and enlarged facet joints. The enlarged facet joints are called ‘facet joint hypertrophy’ and reduce the size of the spinal canal.
- Degenerative longitudinal ligament: The longitudinal ligament is one the ligaments at the back of the spine that holds the vertebrae together. With the normal ageing process and wear and tear, these ligaments become enlarged (called ligamentum flavum) and bulky and like with the degenerate discs and facet joints, they reduce the space in the spinal canal.
The result of these degenerate changes is narrowing or ‘stenosis’ of the spinal canal and less space for the spinal cord and nerves.
2. Spondylolisthesis
A spondylolisthesis is a ‘slip’ of one vertebra over the top of the vertebra below and is most commonly due to degeneration of the pair of facet joints between the two affected vertebrae. Degenerative spondylolistheses occur with age and most commonly occurs at the L4/5 level. The slip can lead to narrowing of the spinal canal.
Spondylolithesis is also often associated with a degenerate disc bulge, enlarged facet joints and enlarged ligaments which lead to further narrowing of the spinal canal.
3. Trauma and fractures
Accidents, falls and other trauma can cause dislocations or fractures (including osteoporotic fractures) of one or more vertebrae. A ‘propulsed fracture’ can cause bone from the fractured vertebra to protrude into the spinal canal and once again reduce the space in the canal and press on the spinal cord and nerves.
Much less common causes of spinal stenosis include:
- Pagets Disease (a bone disease that causes bone overgrowth and therefore narrows the spinal canal)
- Epidural Lipomatosis (an abnormal amount of fat is deposited in the spinal canal reducing the available space for the cord and nerves)
- Infection
- Tumour
Symptoms of Spinal Stenosis
Narrowing of the spinal canal can cause compression of the spinal nerves and, depending on the level of the stenosis, also compression of the spinal cord (remember the spinal cord usually ends at about the level of L1 and it then turns into the cauda equina nerves).
Not all patients who have spinal stenosis have symptoms. However for those patients who do have symptoms, compression of the spinal nerves can cause the following symptoms in one or both legs or arms:
- Pain in the legs or arms (often not in the back or neck)
- Reduced sensation or ‘numbness’
- Burning sensation
- Pins and needles or tingling
- Weakness in the legs or the sensation that the legs feel like “jelly” or will “give way” or feel heavy”
- Myelopathy – loss of balance and difficulty walking caused by compression of the spinal cord therefore usually caused by spinal stenosis in the neck.
Most patients do not feel the symptoms when they are resting or sitting. Typically the symptoms start on standing or walking and are relieved by sitting or bending forward. Once they have rested they can usually start walking again.
Another typical sign is when using a shopping trolley. Patients can walk further, without stopping, when leaning forward on a shopping trolley. This is not because the trolley is supporting you, instead it is because when you lean or bend forward, or sit down, the space in the spinal canal is temporarily increased and this creates a bit more space for the nerves.
The cauda equina nerves control the bowels, bladder and sexual function. These nerves can be compressed in spinal stenosis (and with very large disc prolapses) and in rare cases it causes loss of sensation and function of bowel, bladder and sexual function . This is known as Cauda Equina Syndrome (CES) and requires urgent medical attention and often urgent surgery (see section on Cauda Equina Syndrome for more information).
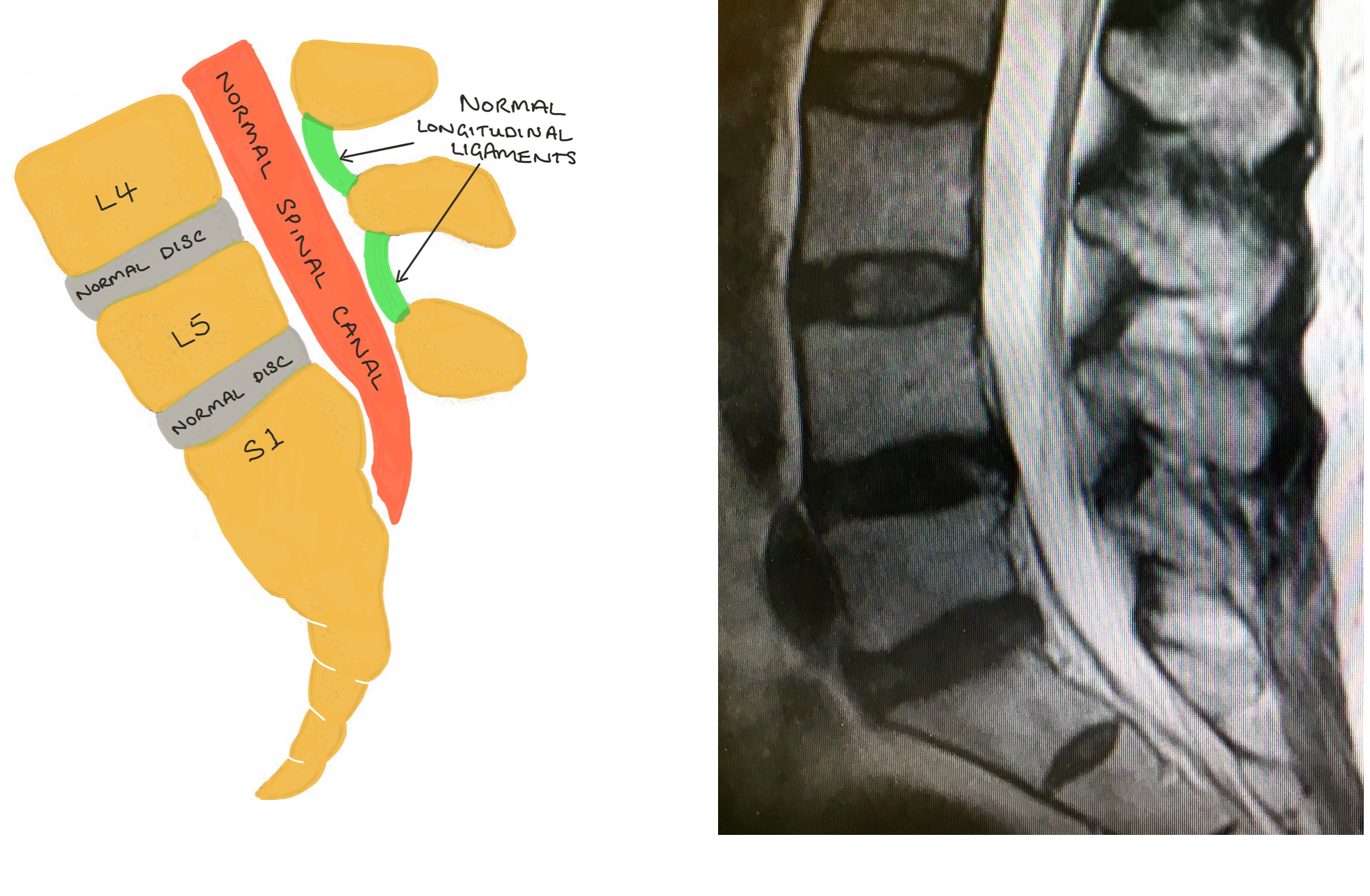
The diagrams and MRI images demonstrate a ‘normal’ spinal canal in the lumbar spine.
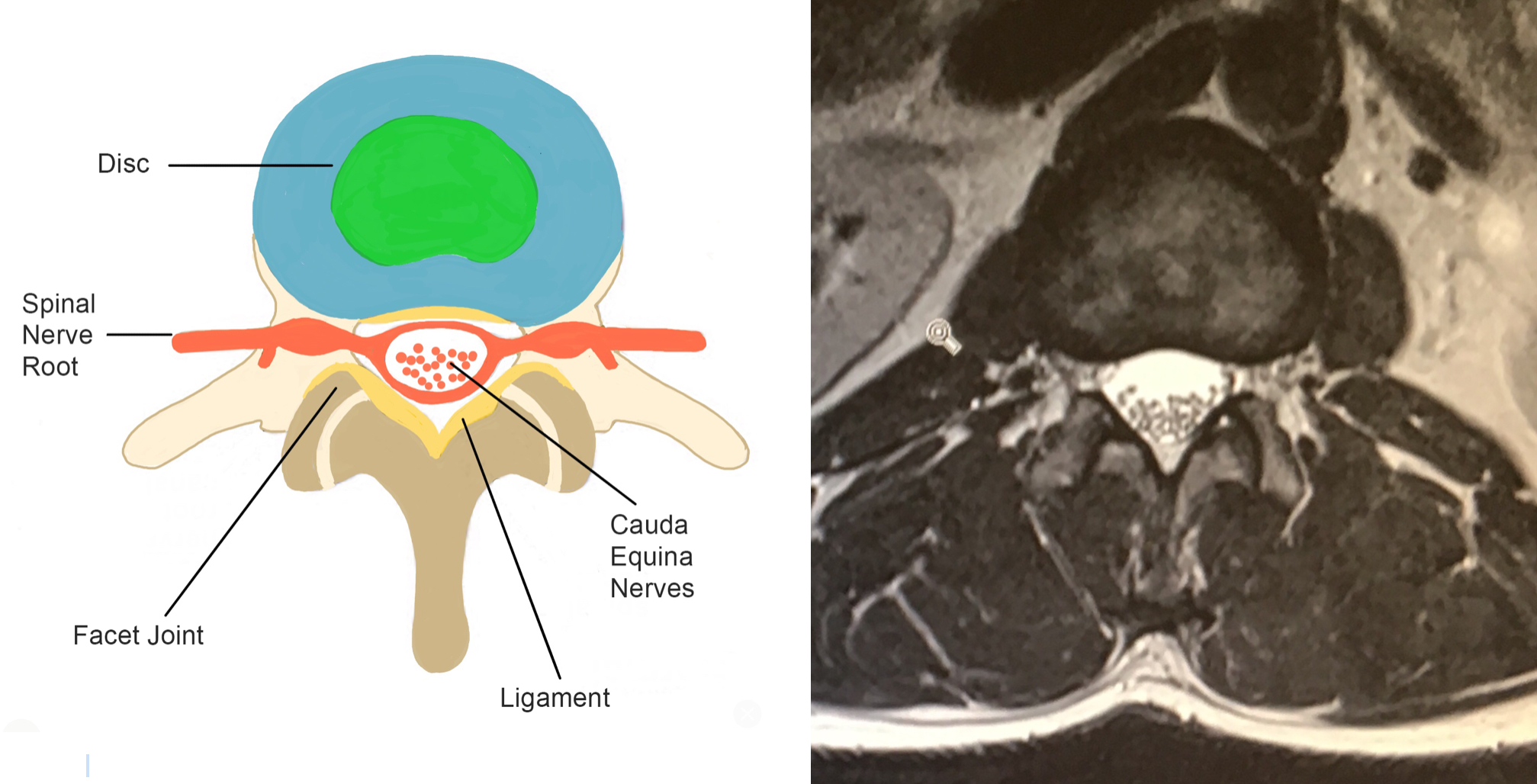
The top images show the lateral (side) view and the bottom images show the corresponding axial (cross-section) of the lumbar spine.
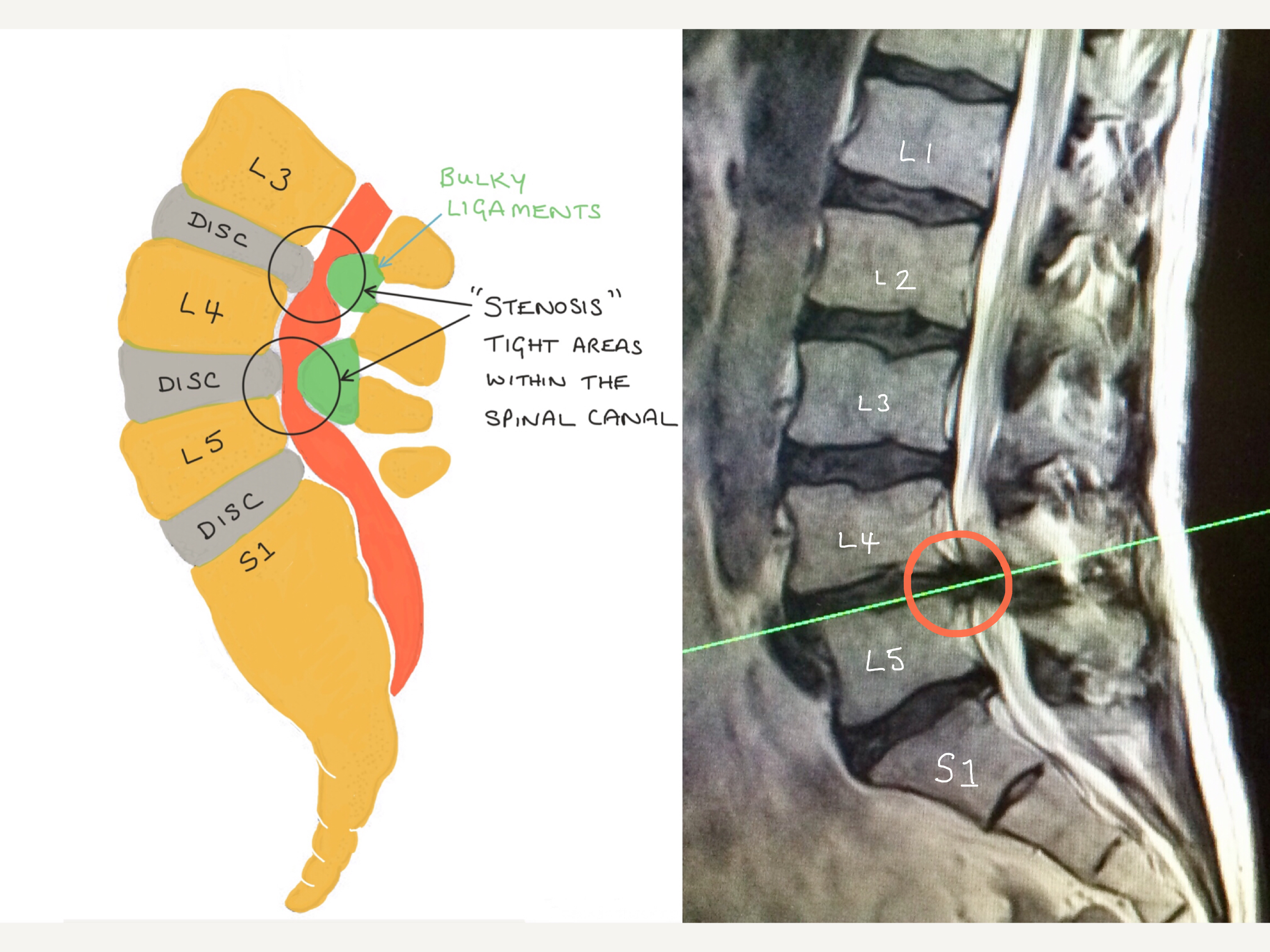
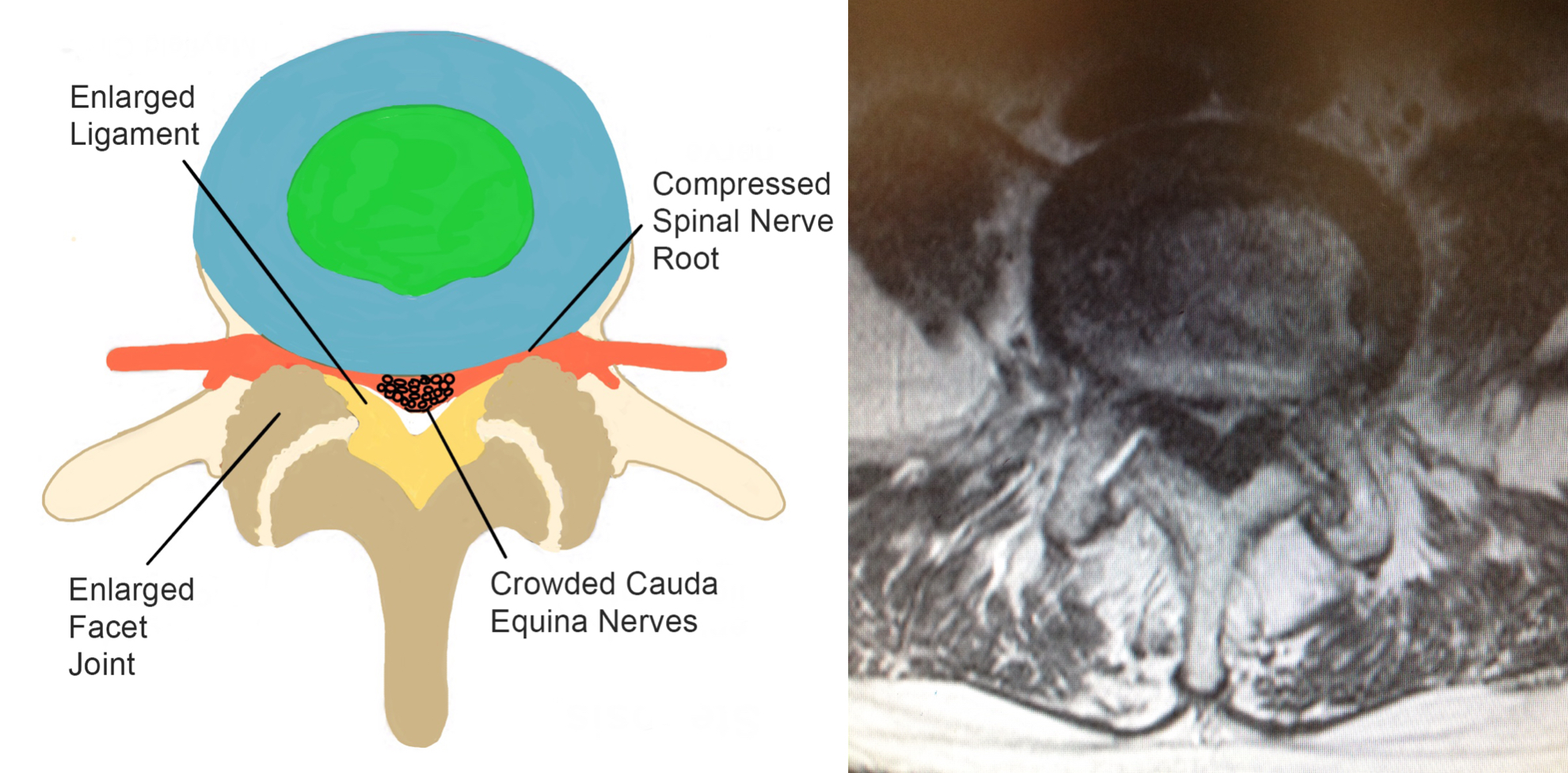
Both Lateral and axial diagrams and MRI images illustrate how a degenerate disc bulge, enlarged facet joints and ligamentum flavum can reduce the space in the spinal canal causing spinal stenosis and resulting in compression of the spinal nerve roots and cauda equina nerves.

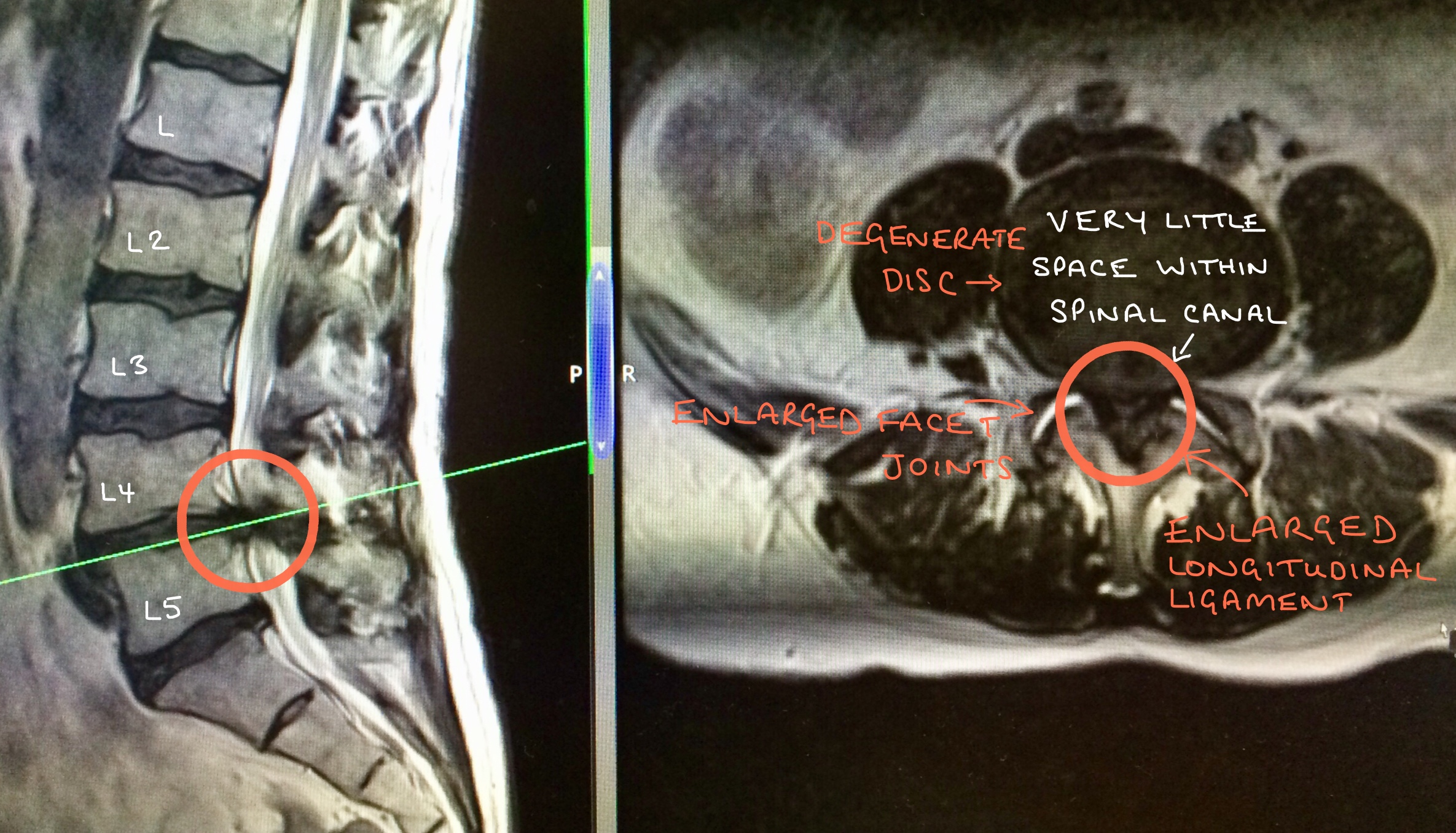
The MRI images above illustrates the side view of the spine, on the left hand side, and the corresponding cross-section, on the right hand side.
The circled areas demonstrate severe spinal stenosis at L4/5 which is caused by a degenerate disc bulge, enlarged facet joints and an enlarged longitudinal ligament.
Diagnosis
Mr Hilton always takes a detailed history and performs a neurological examination as the first of any diagnosis process. Imaging is used usually to confirm, or exclude, a diagnosis and this is generally in the form of standing X-rays, an MRI scan and occasionally a CT scan.
Patients who have symptoms caused by spinal stenosis often tell a similar story; generally no symptoms at rest, instead the symptoms usually start on standing or after walking a certain distance and this distance can vary from only a few metres to a few hundred metres. Pain is not always the main symptom, often the loss sensation or a strange feeling in the legs stops people from from walking. Most patients describe symptoms are relieved when they sit or bend forwards for a few minutes and this allows them to continue walking again before they need to stop and sit/bend forward again.
It is important to remember that although you may have spinal stenosis at one level, the symptoms need to match your MRI scan. For example, stenosis at L5/S1 does not usually cause pain down the front of your thigh as that is more likely to be coming from the L2/3 level.
I also have back pain, is the treatment the same?
The leg symptoms may be associated with back pain. It is important to decide which is the major symptom, back pain or leg pain, as the treatments may be different depending on the predominant problem.
What else could be causing my leg symptoms?
The symptoms of spinal stenosis can be very similar to Vascular Claudication which also causes pain in the legs (and arms) on walking and exercise and stops with rest.
Claudication is a symptom of Peripheral Vascular Disease which causes narrowing of the arteries in the legs (and less commonly, in the arms) resulting in reduced blood flow to the muscles. The symptoms of claudication are usually pain, burning and weakness in the legs on walking and exercise which stops on rest. As it gets worse the pain may also occur at rest and at night and be associated with discoloured skin below the knees and cold feet. These symptoms may be very similar to the symptoms of spinal stenosis (spinal claudication), and tests on the blood supply to the legs may be needed to determine which is causing the symptoms.
Other causes of numbness and altered sensation in the legs and arms include Diabetes or Vitamin B12 Deficiency, both of which can be diagnosed with simple blood tests.
Physical Therapy
Improving spinal mobility, strength and overall fitness may improve symptoms to a manageable level. Pilates, yoga and physiotherapy exercises are important to perform on a regular basis if you can tolerate performing them. Cycling (on a static/exercise bike or on the road) is a very good exercise because patients with stenosis often find this easier than other forms of exercise because the bending forward position temporarily opens up the spinal canal allowing more space for the nerves.
It is important to remember that pain does not always indicate that damage is being done to the spine and you should try and do as much exercise as you can.
Simple, over the counter, pain killers such as paracetamol or ibuprofen may be helpful especially when exercising.
Spinal Injections
X-ray guided epidurals and nerve root blocks can be extremely useful in patients to help to relieve leg pain and altered sensation associated with spinal stenosis. They are also very useful in the diagnostic process and they can confirm or exclude a diagnosis.
Spinal injections have the advantage of being performed under local aneasthetic or sedation and although there are potential risks and side effects, these are extremely rare. As well as being very useful diagnostically, it is estimated that 60% of patients will have significant, long-lasting relief of symptoms and which may be permanent. See section on spinal injections for more information.
Surgery
Without surgery, on average about 60% of patients will symptomatically remain the same and 20% will get worse. However 20% of patients may improve with time or learn to live with and manage their symptoms. Therefore it is very important to be treated for how you are now NOT what you may potentially be like in the future.
If you can manage as you are at the moment then surgical intervention is probably not for you, however if your symptoms are intolerable and significantly reducing your quality of life, despite simpler and conservative treatments, then surgery may be considered. This will also depend upon your general health and fitness.
The aim of surgery is take the pressure off the nerves (and spinal cord) by removing bone and soft tissues, this is known as a spinal decompression. Depending on the initial cause of the spinal stenosis, an instrumented fusion may also be needed.